podiatrist issaquah
Displaying items by tag: podiatrist issaquah
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses the Lapiplasty Bunion Correction

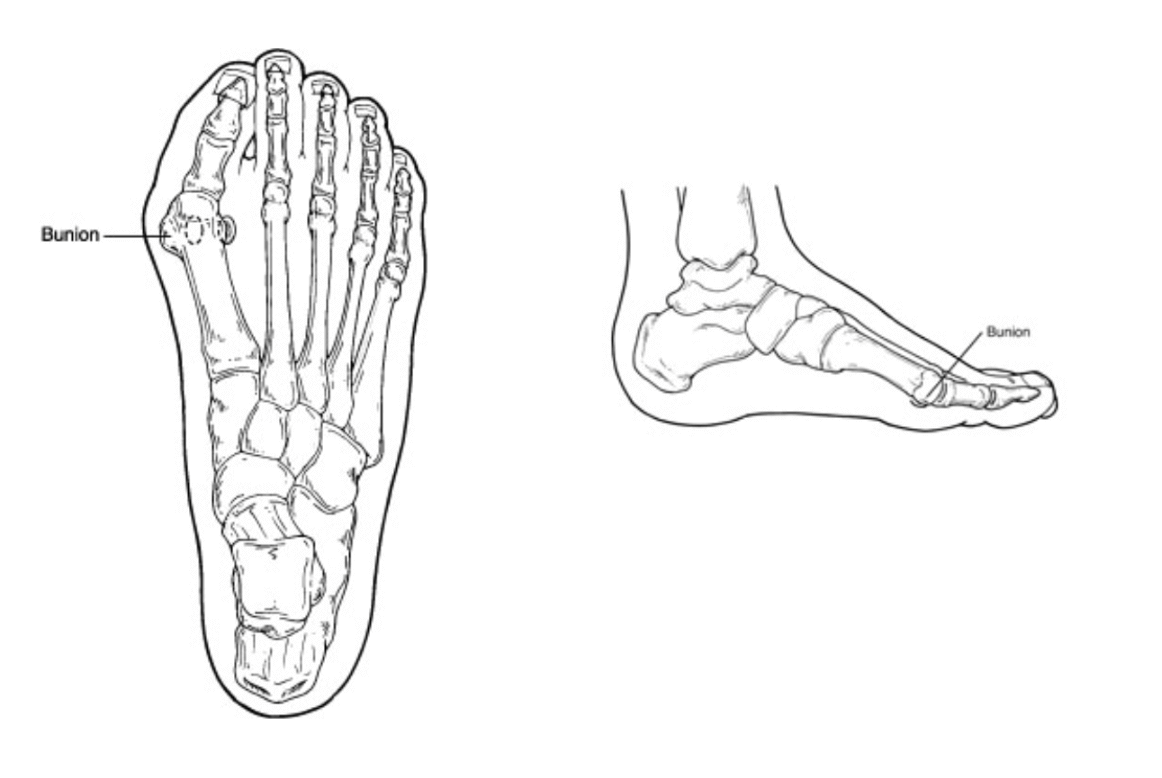
Bunions are painful deformities that are common and can cause pain and discomfort daily. Surgery for bunions has been around for over 100 years but recent advancements have made bunion surgery easier than ever. Today we will discuss the Lapiplasty bunion procedure, its advantages and how it has changed the way we correct bunions.
What is a bunion?
A bunion is an inherited foot issue that involves the deviation of a bone in your foot. Specifically the 1st metatarsal begins to drift in the wrong direction making it difficult to fit shoes and can be quite painful. Genetics play a big role in the development of a bunion and things like shoe gear can contribute to the bunion.
Convention bunion surgery often involves cutting the bone and realigning a joint. This type of procedure has been utilized for years and is still the most popular bunion surgery in the world. It has its applications and is appropriate for certain individuals. The Lapidus or Lapiplasty focuses on larger bunions and people that have a more unstable foot. It aims to correct the bunion in a more comprehensive approach and provides the best long term results.
It involves correcting the bunion in 3 planes, realigning the metatarsal, correcting the bunion at the root cause. The joint where the bunion originates is cut and realigned and fixated to heal in the proper position. Recovery can vary by patient and bone quality same with healing times. I do recommend physical therapy and follow up is essential.
In conclusion Lapiplasty has revolutionized bunion correction and provides excellent long term results and is by far the best procedure for many patients.
If you would like a consultation for your bunion I can help. Call to make an appointment with me at 425-391-8666 or make an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr. Brandon Nelson, A Board Certified Foot Physician & Surgeon, Issaquah’s Top Podiatrist, Discusses the Best Bunion Procedure to Have

I have been practicing medicine now for about 15 years and like to look back from time to time on how it has changed. Currently there is a lot of talk about the Lapiplasty bunion and bunion surgery in general. I thought I would take a few minutes and discuss this topic.
Bunion surgery continues to be one of the most common foot surgeries in the United States if not the most common. I believe the last statistic I read was something like almost 350,000 operations per year. It is hard to believe there are that many bunions out there!
The most utilized bunion surgery is the Austin bunionectomy. This is for a couple reasons. One can correct the vast majority of bunions whether small or large. It has a much faster recovery and is technically not as challenging as other operations. It involves the cutting of the metatarsal head in a chevron pattern and shifting that bone medially. It is usually fixated in place with a few screws. Patients can bear weight immediately and are typically in a walking boot for 4-8 weeks. It has good long term results and will probably continue to be the most common bunionectomy for that reason.
The other most talked about bunion procedure is the Lapidus bunionectomy or the Lapiplasty. This procedure is the choice for very large bunions or juvenile bunions. It is technically more challenging but provides for excellent correction. This involves fusion of the metatarsal cuneiform joint to realign the metatarsal. It usually involves a period of non weight bearing from 3-8 weeks. The long term results are excellent.
That begs the question: which procedure is best for bunion patients? Well the answer is not simple. It really involves a couple key considerations. First being how does the rest of the foot look and how much motion do we have through the 1st metatarsal? Second is patient age and activity level. Third would be overall general health of the patient and bone quality. I recommend seeing a surgeon that performs a lot of bunion surgeries as their outcomes will be better.
If you have a bunion and would like to know your options and have it evaluated schedule, make an appointment with me and I will help you.
Sincerely,
Board Certified Physician & Surgeon
Issaquah’s Top Podiatrist & Foot/Ankle Surgeon
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Issaquah’s Best Podiatrist, Discusses Heel Pain

Heel pain can affect people of all ages, lifestyles and activity levels. You can be an avid exerciser, a home body or just spend all day working on your feet. I will discuss some of the causes of heel pain, the symptoms and when to seek medical attention. I have been a practicing podiatrist in Issaquah for over 25 years and have treated and helped 1000’s of patients.
There are many common causes of heel pain. However a few are the most common and these include; plantar fasciitis, Achilles tendonitis, stress fractures and Baxter’s neuritis.
Plantar fasciitis is caused from an inflammation of a band of tissue running on the bottom of the foot. The job of the fascia is to support the arch of the foot and control 3 dimensional movement. It often occurs with repetitive stress like standing all day or running.
Achilles tendonitis is usually located more towards the back of the heel. The Achilles tendon helps to push off the foot during the gait cycle. Often any activity that increases load like jumping rope can cause the Achilles to become inflamed. People often feel swelling or a thickening of this tendon in the ankle.
Stress fractures are usually related to overtraining and time. They occur with repetitive loading of a bone. The bone I am speaking of in this case is the calcaneus. These can be tricky to diagnose.
Baxter’s neuritis is rare but is often confused for plantar fasciitis. There is usually more of a burning or tingling that occurs. Often there is not an increase in activities and no correlation with time spent on your feet and pain.
I recommend seeking early treatment for heel pain. I see that patients that wait longer have a harder time recovering and often need more therapeutic interventions. This is especially true for athletes, get in early and get a head of the pathology.
If you have heel pain and would like an appointment with Issaquah’s top Podiatrist at 425-391-8666 or make an appointment online.
Sincerely,
Board Certified Foot & Ankle Surgeon
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Issaquah’s Best Podiatrist, Discusses Why Lapiplasty Bunion Correction
Bunion surgery is the most common foot surgery done in the United States. There are many different techniques to correct a bunion. Most involve either cutting of a bone or fusion of a bone. All involve realignment of a joint in order to improve the function and appearance of the foot.
I have now been practicing medicine and surgery for over 15 years. I am a podiatrist in Issaquah and have had the opportunity to help 1000’s of patients with bunions. Bunions can be extremely painful and the majority of people will require them to be fixed at some point. This experience has led me to utilize Lapiplasty on the majority of my patients.
Why the Lapiplasty?
1. It provides correction at the center of a bunion deformity
2. It has been proven to have the best long term outcomes
3. It stabilizes the foot structure
4. It does an excellent job for large bunions
5. It has been utilized for over 100 years
I encourage anybody with a bunion to get evaluated by a surgeon that performs a significant amount of bunion corrections annually. Experience can make a big difference in outcomes and the Lapiplasty is a technically difficult procedure to execute. If you have a bunion and would like to discuss the Lapiplasty make an appointment with Issaquah’s top Podiatrist at 425-391-8666 or make an online appointment.
Sincerely,
Board Certified Foot & Ankle Surgeon
Dr. Timothy Young discusses a different kind of bone spur in the foot: Enthesophytes, not your typical bone spur.

Dr. Timothy Young discusses a different kind of bone spur in the foot: Enthesophytes, not your typical bone spur.
Introduction:
There can be confusion when talking about bone spurs in the foot. In general, when one thinks of an arthritic bone spur, that is often an osteophyte. However, there is a different kind of bone spur; this is an enthesophyte. The best way to think of an enthesophyte is calcification of the tendon or ligament at its attachment to the bone. A common example would be a heel spur related to plantar fasciitis or calcification of the Achilles tendon where it attaches to the back of the heel bone. It is important to know, however, that calcification of the Achilles tendon or a plantar calcaneal heel spur, in either case, may not cause any pain or symptoms at all. On the other hand, if there is associated inflammation or degenerative changes, there may be symptoms and pain.
Enthesopathy is another similar term describing this condition. Note that Enthesopathy often occurs in response to a mechanical condition, but there can be more of a systemic inflammatory condition also, such as ankylosing spondylitis or psoriatic arthritis. Some of the autoimmune arthritic conditions may potentially be related to this condition.
Enthesophytes vs. Osteophytes: An Overview
Enthesophytes Defined: Enthesophytes are abnormal bony projections that occur at the attachment points of tendons or ligaments to the bone. These bony outgrowths are the result of the body's response to chronic stress and irritation in these connective tissues.
Osteophytes in Contrast: We have previously discussed osteophytes in our prior blog. Osteophytes are abnormal bony projections that form within joint spaces. Unlike enthesophytes, which are associated with the insertion points of tendons and ligaments, osteophytes develop as a response to joint degeneration and inflammation, often associated with conditions like osteoarthritis. The most common osteophytes in the foot and ankle could include the great toe joint, where bone spurs limit motion and cause an enlargement on the top of the joint. In the ankle, it is often the front of the ankle joint that develops osteophytes that can also limit ankle joint motion.
The Stress Response: Understanding Enthesophyte Formation
Chronic Tendon or Ligament Stress: Enthesophytes are born out of the repetitive stress and strain on tendons and ligaments. This stress can result from various factors, including overuse, improper biomechanics, or inflammatory conditions affecting the connective tissues.
Microtrauma and Inflammation: Microscopic damage to the tendon or ligament can lead to localized inflammation. As the body attempts to repair this damage, the bone responds by forming additional bony tissue at the insertion point – thus, an enthesophyte is born.
Common Locations: Enthesophytes can occur at multiple sites throughout the body. Common examples in the foot include the heel, with two common examples being Achilles enthesophyte and an enthesophyte associated with plantar fasciitis or the most typical heel spur.
Distinguishing Features: Enthesophytes vs. Osteophytes
Location:
Enthesophytes: Develop at the attachment sites of tendons or ligaments to bones.
Osteophytes: Form within joint spaces in response to joint degeneration.
Associations:
Enthesophytes: Linked to chronic tendon or ligament stress and inflammation.
Osteophytes: Associated with joint degeneration and conditions like osteoarthritis.
Clinical Manifestations:
Enthesophytes: May cause localized pain at the attachment sites, especially during movement.
Osteophytes: Can impact joint movement, causing pain, stiffness, and reduced range of motion.
Managing Enthesophytes: It is important to understand that in many cases, it is really because of the enthesopathy that we are treating so for calcification of the Achilles tendon, we often are treating Achilles tendon problems. And for treating a plantar calcaneal spur, we often are treating plantar fasciitis as the primary problem, and the enthesopathy may be a secondary problem.
Conservative Measures:
Rest, activity modification, and gradual return to exercise.
Physical Therapy: Stretching and strengthening exercises.
Anti-Inflammatory Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs) to manage inflammation and pain.
Orthotic Support:
Proper footwear and orthotic devices to alleviate stress on affected areas.
Shockwave Therapy: This is extremely effective at treating Achilles tendon problems and calcific Achilles insertional tendinosis and plantar fasciitis.
Platelet Treatments: Concentrated platelets are injected into the damaged tendon or plantar fascia.
Surgical Procedure Interventions:
Tenex: This is a less invasive type of procedure that can remove damaged tendon and remove some of the calcified portions.
Traditional Surgery: In resistant cases, surgical direct treatment may be considered.
Conclusion:
Enthesophytes may relate to the body's adaptation to the demands placed on tendons and ligaments. This condition may (or may not) cause discomfort, especially in the presence of chronic stress, and may limit exercise. Understanding their distinct nature and differentiating them from osteophytes is crucial for accurate diagnosis and effective management. If you suspect the presence of enthesophytes and experience persistent pain or discomfort, please contact our office for consultation or make an appointment online.
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Why He Has Been Doing the Lapiplasty Procedure for over 15 years

Bunions are an inherited foot deformity that can be exasperated by shoe gear and activities. They are created when your first metatarsal begins to shift out of place to stabilize your foot. They usually become worse with time and eventually cause pain and discomfort. Many patients require surgical intervention.
The surgical correction of a bunion can have great outcomes and provide long lasting benefits. In the United States there are many different approaches to correction of a bunion. I have been operating long enough to have had experience in most of these procedures. That is why my bunion correction of choice is Lapidus or Lapiplasty.
The Lapidus or Lapiplasty is a procedure that dates back almost 100 years. It was first described by Dr Lapidus and to date has stood the test of time for bunion correction. It involves utilizing a fusion of 2 bones at the apex of the bunion or where the bunion starts. This provides dynamic correction and great long-term stability. I find patients are happy with their new foot structure and often want the other side fixed as well.
If you have been contemplating bunion surgery, give me a call. I have an onsite surgery center that saves time and money. IV sedation provides for a great experience. If you would like a consultation for your bunion I can help. Call to make an appointment with me at 425-391-8666 or make an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses the Best Options for Bunion Surgery
.jpg)
Bunions are present in many different sizes and shapes. I see bunions on the inside of the foot, the outside of the foot and both. It is important to remember that some small ones can be painful, and some large ones can be pain free. It often seems to be dependent upon activity levels and shoe gear. If they hurt or limit your lifestyle then maybe it is time to fix them.
Fixing your bunion
Bunion surgery has two main procedures that are done. One is what is called a head procedure. This is basically cutting the bone and realigning it through transposition of the bone. Usually fixated with one or two screws. The other involves fusion of a joint, specifically the joint that is involved with the creation of the bunion. This procedure is called a Lapidus bunionectomy.
Bunion recovery
Recovery really depends on the procedure that is performed. Head procedures recover faster and usually involve no periods of non-weight bearing. The fusions often involve a period of crutches or knee scooters. This can be as short as 3 weeks or as long as 10 weeks. The weight bearing status can be dictated by other procedures that are done as well.
Which bunion surgery is right for me?
This is a hard question to answer. I believe this is where your consultation with your surgeon is extremely important. Other factors like lifestyle, recovery support, expectations and experience can play a major role. I think it is important to get an entire overview of the process and have a discussion with your surgeon.
If you would like a consultation for your bunion I can help. Call to make an appointment with me at 425-391-8666 or make an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Plantar Fasciitis

Plantar fasciitis affects millions of people worldwide. It is often a debilitating condition that limits people’s activities. It is characterized by pain in one’s heel, pain when we get out of bed or can even be a bruised sensation to the bottom of the foot. Today I will discuss some of the causes, symptoms, diagnosis, and treatment. The plantar fascia itself is a thick ligament like tissue that runs on the bottom of the foot to provide support.
Causes:
The number one cause is overuse. This can be exercise or standing all day or a change in the amount of either of these. Other causes can be shoe gear, weight or even the foot structure one is born with.
Symptoms:
The most common symptom is sharp heel pain, especially when you first get up from a seated position. This usually improves as we walk but returns at the end of the day. Some people experience stiffness or even burning.
Diagnosis:
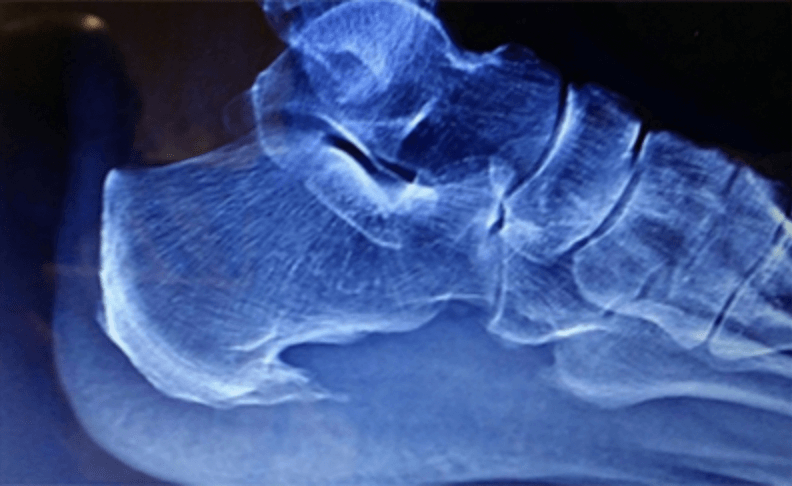
A good clinical examination can help identify plantar fasciitis for most people. The is usually pain with palpation of the heel, specifically at the heel bone where the fascia attaches. An x-ray can be useful to detect bone spurs.
Treatment:
The mainstay of treatment is to work on stretching of the foot and Achilles. Additionally, increasing support for the feet can be helpful. Often by the time I see patients an injection is needed to calm down the inflammation and help with recovery.
If you would like a consultation on your heel pain, I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
Dr Brandon Nelson
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Heel Pain and When to See A Foot & Ankle Specialist

Are you currently suffering with heel pain? I can remember those days not long ago for me. I would wake up in the morning and that first step pain was terrible. It would take a couple minutes and it would finally loosen up only to return every time I sat down. Does this sound familiar? If so, you probably have plantar fasciitis. The big question is when to see a foot and ankle specialist, the answer is now.
The sooner you get in to seek treatment the faster your recovery will be. With procrastination the inflammation gets worse, and you will take longer to recover. I tell all my patients the sooner we initiate treatment the faster we can get you back to enjoying the things you like.
Treatment of plantar fasciitis usually starts with a review of your activities. What are you currently doing for exercise and how often? Have there been any recent changes? I like to get an x-ray to check for bone spurs and arthritis. A good overall examination of the foot structure and lower leg can be helpful along with any treatments that have been tried. If the diagnosis is still plantar fasciitis then the average patient I see will be about 50% better in less than a week with the first line of therapy.
If you have heel pain, you know how uncomfortable it can be. If you would like a consultation on your heel pain, I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
Dr Brandon Nelson
Dr. Timothy Young, a Board-certified Foot Surgeon discusses bone spurs in the foot: Osteophytes
Dr. Timothy Young, a Board-certified Foot Surgeon discusses bone spurs in the foot: Osteophytes
Defining Osteophytes: Osteophytes, a subset of bone spurs, are characterized by the outgrowth of new bone on the margins of a synovial joint. They often develop in response to joint degeneration and are associated with conditions like osteoarthritis.
Locations of Foot Osteophytes:
1. Joints: Osteophytes often form on the margins of joints of the foot, impacting movement and causing pain.
2. Edges of Bones: They may also develop along the edges of bones, affecting the alignment of joints.
Causes and Risk Factors:
1. Joint Degeneration: Osteoarthritis, a common cause of bone spurs, leads to the breakdown of cartilage and prompts the body to form osteophytes.
2. Repetitive Stress: Continuous mechanical stress on specific areas of the foot, often due to poor biomechanics or ill-fitting footwear, can contribute to the development of bone spurs. This often involves the force of gravity on weight-bearing joints. A good example would be the ankle joint.
Symptoms and Diagnosis:
1. Pain: Persistent pain in the affected area, especially during movement or weight-bearing activities.
2. Reduced Range of Motion: Difficulty moving the affected joint due to the presence of bone spurs.
3. Visible Bumps: In some cases, visible or palpable bumps may be present, indicating the presence of bone spurs. A good example this would be a bump on the top the midfoot that is due to large osteophytes in this location.
4. X-rays and ultrasound: x-rays and ultrasound can show the osteophytes. It is usually not necessary to do an MRI or CT scan.
Treatment Options:
1. Conservative Measures:
- Rest, ice, compression, and elevation (R.I.C.E.).
- Orthotic inserts and supportive footwear.
2. Physical Therapy:
- Stretching and strengthening exercises.
- Therapeutic modalities to alleviate pain and inflammation.
3. Medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain management.
4. Injections: injections can deliver medication such as Supartz which is a synthetic joint lubricant. This was originally FDA approved for the knee but is now used throughout the body. For the foot and ankle, it is most commonly used in the ankle joint and the great toe joint. Cortisone is not used as often, since repetitive use can weaken the existing Cartledge and adjacent joint capsule.
- In severe cases, surgical removal of the bone spur may be considered, or in some cases the joint can be stabilized by fusing it or placing an implant in the joint.
Conclusion:
Bone spurs and osteophytes in the foot can present challenges, but with proper understanding and timely intervention, individuals can manage their symptoms effectively. If you suspect the presence of bone spurs in your foot, please contact our clinic and we can review your options.



