podiatrist issaquah
Displaying items by tag: podiatrist issaquah
Dr Brandon Nelson, a Board-Certified Physician and Surgeon, Discusses What His Patients Experience After Bunion Surgery

I have now been operating for about 15 years and can tell you bunion surgery has really changed. In the average week I correct 3-5 bunions and have now operated on 1000’s of bunions. Some bunions are small, and some are large and very complex, but all can be fixed. I continue to learn and research new techniques, and these have afforded me opportunities and skills to provide great outcomes and minimal down time.
In the past bunion surgery was done at the hospital and often required and overnight stay. Patients were placed in casts and often non-weight bearing for months. I have heard stories of patients being uncomfortable for weeks.
I can tell you techniques have changed, and I am happy to outline how the average patient experience goes at my clinic. My clinic has an onsite surgery center that provides a huge cost and time savings as compared to a free-standing surgery center or a hospital. Most bunion cases are completed in under 3 hours from the time one enters the clinic to when ones leaves. We utilize IV sedation which is safer and allows me to perform a nerve block for long term pain relief. Pain medication is only needed for a few days and many patients do not even take anything apart from an NSAID. Weight bearing status depends on any ancillary procedures, but most bunion patients can walk immediately after surgery.
If you have bunion and have been contemplating having it fixed make an appointment today and I will review your options and help you make an informed decision.
Sincerely,
Dr Brandon Nelson, A Board-Certified Physician and Surgeon, Discusses Options to Treat Neuromas
Neuromas of the foot are common in woman between the ages of 40-60. The typical neuroma will present with pain, burning and tingling to the forefoot. Most people state the pain feels better without shoes and rubbing one’s foot can help. There does not need to be a history or trauma or even previous foot pain to have a neuroma.
The neuroma itself is usually located in the 3rd interspace of the foot. This is between the 3rd and 4th toe and can be either right or left foot and rarely both feet. The reason this is the most common spot is the fact two nerves come together in this location. Often this creates an entrapment as this location can have limited space.
Treatment options for neuromas range from stretching and icing to injections and orthotics. Rarely now is surgery required as the conservative measures are so successful. I typically employ a prescription orthotic in conjunction with a series of alcohol injections. I have developed a protocol over years of treating thousand of patients and this has proved so successful that I rarely find surgery needed. I even see quite a few patients that have seen multiple other providers. If you want to avoid surgery and have a neuroma I can help. I look forward to getting you back on the road to recovery, Dr. Brandon Nelson, Board Certified Physician and Surgeon.
Give us a call at 425-391-8666 or make an appointment online today.
My Heel is Sore All the Time!

Heel pain continues to be the most common reason a person visits the foot and ankle doctor or podiatrist. For us it constitutes about 1 out of every 4 patients and is one of the most important things we treat. We specialize in heel pain and have seen tens of thousands of patients for it. Our success rate with conservative measures to get rid of heel pain is close to 99%, very few people require surgical intervention.
Plantar fasciitis continues to be the number one cause of heel pain. Most people will get pain first things when they get out of bed in the morning or after standing for long periods. It is common for some with fasciitis to not have morning pain. There also is a correlation with a new exercise program and the development of plantar fasciitis. I always recommend getting in early to see us as it is much easier to treat early on.
Bursitis is another very common cause of heel pain. We often see this in a high arched foot or a runner. Patients will have symptoms like plantar fasciitis but usually on ultrasound we can see the bursal sack. Bursitis usually responds very well to the treatment program we provide and very few people need to sideline their activities.
Nerve entrapments can also create heel pain. This is usually a nerve called Baxter’s nerve. Most people will experience a lot of burning and tingling with this condition. However, this can be a tricky diagnosis and may require special testing. This condition can respond well to a steroid injection adjacent to the nerve.
If you are experiencing heel pain we are here to help give us a call at 425-391-8666 or make an appointment online today.
Dr Timothy Young Talks About Tight Calves and Foot Problems, Part 2
Tight calves and Achilles are a major factor in many foot problems. That is why we use a night splint and calf stretching is helpful for many problems. Problems in the front of the foot like 2nd toe capsulitis metatarsalgia often respond well to calf stretching. We have discussed how during gait, early heel rising and transfer of weight to the front of the foot can increase the load and weight transfer to the forefoot (and midfoot). This early transfer of weight and mechanical load can be destructive.
With our example of capsulitis of the 2nd toe, we now have an extra load going through the 2nd metatarsal and toe joint. Eventually the extra load can strain the 2nd metatarsal and capsule. This can lead to capsulitis or even a stress fracture of the metatarsal. So, to help with this, we have our patients stretch their calf and use a night splint. We avoid shoes that further put more pressure on the front of the foot (like high heeled shoes). We even recommend shoes with zero heel drop, like Altra shoes. This is just one example of how equinus can factor into a foot problem, there are so many more examples where this happens. So, this is just the “tip of the iceberg” as a major factor in many foot problems and pathology. Keeping your calf stretched out is one of the single best exercises you can do to keep your feet healthy!
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr Timothy Young Talks About Tight Calves and Foot Problems
Dr Timothy Young Talks About Tight Calves and Foot Problems
As mentioned, the mechanical load on the foot from the calf and ultimately the Achilles is tremendous. So, with equinus ( a tight calve and or Achilles) there are many problems. Think of a woman who wears high heel shoes every day for many years and over time the calf gets less flexible. Now with that tight calf, her gait has changed. As she walks, with each step going forward that tight calf pulls, and her heel comes off the ground early. Early heel off with gait leads to early transfer of weight and force to the front of the foot. Over time, this extra pressure on the front of the foot can cause problems. This is like the childhood toewalker, but with adult body size and weight.
If you are experiencing any foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr Brandon Nelson, A Board Certified Surgeon, Discusses Ankle Surgery
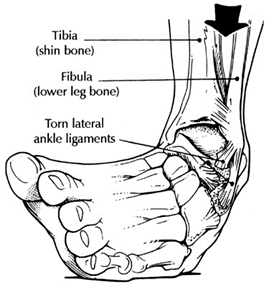
Surgery of the ankle is a fairly common procedure. The majority of ankle surgeries have to do with the outside of the ankle or the lateral ankle complex. The lateral ankle complex is composed of the lateral ankle ligaments and the peroneal tendons. The ligaments on the outside of the ankle are the most important ligaments for stability. These ligaments are often injured with an ankle sprain or ankle fracture. The peroneal tendons work to dynamically stabilize the ankle with activities. These tendons can also be injured with repetitive use or chronic ankle sprains. It is important for anybody that has more than 1 ankle sprain a year to have the structural integrity of their ankle evaluated.
Evaluation of the ankle usually involves and x-ray and a physical examination. In addition, I will often order and MRI to get a better appreciation of the structural components of the ankle. I like an MRI because one can see what the ligaments and tendons look like. This is extremely helpful for evaluation of what needs to be repaired for surgery and what the tissue consistency looks like for the repair.
The surgical procedure itself, or the repair, can be relatively straight forward as in just a ligament stabilization or more complex included bone work. The most common ankle procedure is the lateral ligament reconstruction or the Brostrum procedure. This is a great procedure for anybody with chronic ankle sprains. With this procedure there is a chance you may need the tendons repaired as well.
If you are experiencing frequent ankle sprains or have pain on the outside of the ankle I can help. Make an appointment today and we will get you back on the road to recovery. Give us a call at 425-391-8666.
Dr. Timothy Young Discusses Stubborn Capsulitis Part 2

Again, I have had this problem before and as mentioned in prior blogs I did many of the appropriate initial treatments listed in my previous blogs. The next step to consider is some of the other alternative treatments. We used to do cortisone injections for this, and we do that very rarely now. There is a non-cortisone anti-inflammatory called Injectable Sterile Traumeel that has much decreased potential risk for damaging the capsule (unlike cortisone). There is also PRP–platelet rich plasma. This can be very effective especially when combined with shockwave treatment. Shockwave treatment can also be done as a stand-alone procedure. The problem with some of these additional treatment options is that they often take several months to really be effective. That's where it's hard to do this but one needs to have patience. Again, that's where cross training can be helpful such as cycling or aqua jogging. For my capsulitis as mentioned, I did the typical initial treatments. I wore special orthotics modified for the capsulitis, I have shoes with a good rocker design, I don't go barefoot at home. I work on stretching my calf and I have a night splint . I stopped running for exercise and only did walking.
Dr. Timothy Young Discusses Stubborn Capsulitis

I have had this condition myself. We are talking about capsulitis of the second metatarsal phalangeal joint (MTP joint) in the ball of the foot, near the base of the second toe. There have been previous blogs about the potential cause of this problem. Treatment has to address the underlying cause and foot structure as much as possible. If the calves are tight, then they have to be stretched and use a night splint or even have a gastroc recession surgery. If there is a bunion and the whole first metatarsal is not bearing is fair share weight then it can cause stress overload to the next in line second metatarsal. Orthotics and foot taping often help this.
Sometimes it's not enough and sometimes especially if there is damage to the capsule such as the plantar plate, we then have to correct the bunion and consider surgery on the second metatarsal. But there are other cases that don't require surgery. It still imperative to do all the other treatments. The correct shoes with a forefoot rocker, sometimes zero drop shoe such as Altra Shoes can also help. Avoiding the activity that seems to aggravate this also can be critical. For example, if you're runner or speed walker, you may have to put that on hold or do cross training until her symptoms have completely resolved. For myself, this seemed to come on after I had resumed running after several months off. I had to make sure my orthotics were still appropriate for this problem. I wore correct shoes. I had to stop running and cross train. I worked on stretching my calf and I have a night splint also.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr Brandon Nelson, A Board Certified Surgeon, Discusses How To Get Rid Of That Morning Foot Pain

It is common for patients to come in the office and relate pain in the morning or right when they get out of bed. This can be a challenging way to start your day and can lead to chronic foot pain. Most patients describe the pain as a bruised feeling to the heel or a tightness with pins and needles. This can go on for months and become chronic. The most common cause of this type of pain is Plantar Fasciitis. Plantar Fasciitis is an inflammation of a supporting band of tissue on the bottom of the foot. The Plantar Fascia is essential for normal foot function and when it is inflamed daily tasks can be overwhelming.
Morning pain is one of the most common signs of Plantar Fasciitis. The reason behind this is while you sleep your Fascia and Achilles Tendon have a chance to relax. With this relaxation both structures begin to tighten up. This tightening up leads to stiffness when you first step on your foot. One can really help this by exercising their foot before getting out of bed. I recommend writing the alphabet with your foot and stretching with a theraband.
If your pain continues for more than a week an appointment is essential. Give us a call at 425-391-8666 or make an appointment online today.
Dr. Brandon Nelson Discusses Heel Pain

Heel pain can be extremely frustrating and challenging to treat. It is most often caused by plantar fasciitis, bursitis, or a stress fracture. It is important to find out the underlying cause before treatment and I highly recommend seeing a foot and ankle specialist before initiating and sort of treatment.
Bursitis, this is basically and inflammation of a sac that is used to cushion the foot. Typically, you will have similar symptoms to plantar fasciitis. Patients experience pain in the morning or with standing and after rest. It can be hard to differentiate from plantar fasciitis. However, at our clinic we have an ultrasound unit which we can use to visualize the bursa and help initiate treatment.
Stress fractures are usually seen after one begins to exercise. There can be accompanying swelling and stiffness. This pathology hurst constantly and can lead to a complete fracture. It is vital to get an x-ray and confirm the diagnonsis.
Heel pain or plantar fasciitis is the most common cause and can be variable in presentation. Classically, patients experience pain in the morning that gets better with a few steps. Most patients have increased activity levels and find pain returns whenever they rest and get us. There is a direct correlation with early intervention and a shorter duration of symptoms. I highly recommend getting in as early as possible to see your foot and ankle physician.
If you are suffering with heal pain I can help, come see me today. Give us a call at 425-391-8666 or make an appointment online today.



