podiatrist seattle
Displaying items by tag: podiatrist seattle
Dr. Timothy Young, a Board-certified Foot Surgeon discusses bone spurs in the foot: Osteophytes
Dr. Timothy Young, a Board-certified Foot Surgeon discusses bone spurs in the foot: Osteophytes
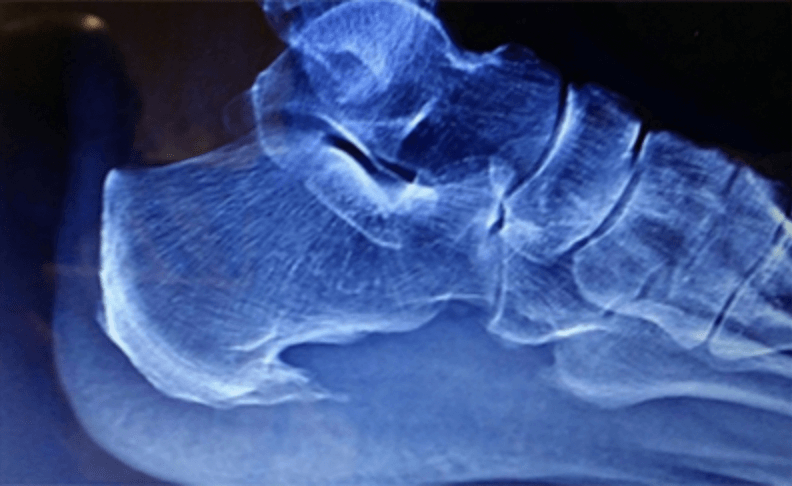
Defining Osteophytes: Osteophytes, a subset of bone spurs, are characterized by the outgrowth of new bone on the margins of a synovial joint. They often develop in response to joint degeneration and are associated with conditions like osteoarthritis.
Locations of Foot Osteophytes:
1. Joints: Osteophytes often form on the margins of joints of the foot, impacting movement and causing pain.
2. Edges of Bones: They may also develop along the edges of bones, affecting the alignment of joints.
Causes and Risk Factors:
1. Joint Degeneration: Osteoarthritis, a common cause of bone spurs, leads to the breakdown of cartilage and prompts the body to form osteophytes.
2. Repetitive Stress: Continuous mechanical stress on specific areas of the foot, often due to poor biomechanics or ill-fitting footwear, can contribute to the development of bone spurs. This often involves the force of gravity on weight-bearing joints. A good example would be the ankle joint.
Symptoms and Diagnosis:
1. Pain: Persistent pain in the affected area, especially during movement or weight-bearing activities.
2. Reduced Range of Motion: Difficulty moving the affected joint due to the presence of bone spurs.
3. Visible Bumps: In some cases, visible or palpable bumps may be present, indicating the presence of bone spurs. A good example this would be a bump on the top the midfoot that is due to large osteophytes in this location.
4. X-rays and ultrasound: x-rays and ultrasound can show the osteophytes. It is usually not necessary to do an MRI or CT scan.
Treatment Options:
1. Conservative Measures:
- Rest, ice, compression, and elevation (R.I.C.E.).
- Orthotic inserts and supportive footwear.
2. Physical Therapy:
- Stretching and strengthening exercises.
- Therapeutic modalities to alleviate pain and inflammation.
3. Medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain management.
4. Injections: injections can deliver medication such as Supartz which is a synthetic joint lubricant. This was originally FDA approved for the knee but is now used throughout the body. For the foot and ankle, it is most commonly used in the ankle joint and the great toe joint. Cortisone is not used as often, since repetitive use can weaken the existing Cartledge and adjacent joint capsule.
- In severe cases, surgical removal of the bone spur may be considered, or in some cases the joint can be stabilized by fusing it or placing an implant in the joint.
Conclusion:
Bone spurs and osteophytes in the foot can present challenges, but with proper understanding and timely intervention, individuals can manage their symptoms effectively. If you suspect the presence of bone spurs in your foot, please contact our clinic and we can review your options.
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses ForeFoot Pain or Pain In The Front Of One’s Foot
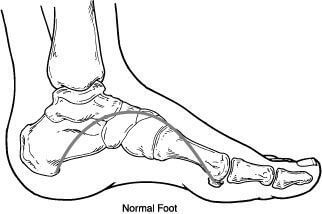
The front of your foot or the area where your toes begin is called the forefoot. This area consists of your toe bones, your phalanges and your metatarsals, the long foot bones. This area is where you push off when ambulating and provides stability for forward propulsion. This is a complex anatomical area and more than a few pathologies can exist in this location but I will discuss a few of the most common. These include neuromas, capsulitis and stress fractures.
Neuromas are an entrapped nerve that can cause burning and tingling. These usually occur in the 3rd interspace. Most patients have a sensation that is electrical and is worse in shoes and relieved by taking off their shoes and rubbing the forefoot. These seem to be more common in women than men and especially around the 4th-6th decade of life. Neuromas have some great treatment options available one of most successful is dehydrated alcohol injections. The success rate with these injections approaches 89%.
Capsulitis is a term we use to describe inflammation of a joint. This most commonly occurs in the metatarsophalangeal joint of the foot. We tend to see this in a patient with a bunion or high arched foot. The main cause seems to be a biomechanical imbalance. It is important to get an x-ray with capsulitis as arthritis can have a similar presentation.
Stress fractures usually present with swelling. They often occur as one begins a new training program and can cause pain for weeks. Typically these will be relieved with rest and exacerbated by activity. Most will heal with a change in activities and calcium supplementation. However again an x-ray is warranted to rule out other pathologies and to monitor healing.
If you are having forefoot pain I can help. Schedule an appointment with Dr Brandon Nelson, give us a call at 425-391-8666 or make an appointment online.
Sincerely,
Board Certified Physician & Surgeon
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Achilles Tendonitis
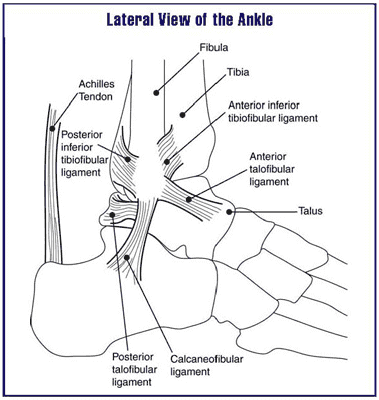
Many athletes will suffer from the dreaded Achilles tendonitis. Increased training and often a change in activities can precipitate this pathology. It is quite frustrating and can sideline many active patients. I personally have dealt with this issue and can understand the challenges associated with it.
The Achilles tendon is the main unit in the lower extremity for the push off phase of gait. It contracts and helps individuals with forward motion. It is constantly under load and being utilized with every step. It is a wonder that more people don’t suffer from tendonitis.
The main cause continues to be overuse. It often is seen in runners and joggers and triathletes. In my office, runners seem to suffer from it. Runners seem to have the biggest demand on this tendon and overuse is quite easy. However, they are not the only one’s, basketball players seem to be affected as well. Probably related to the loading requirements of jumping. Regardless of the causes, it is important to seek help early in the process.
Early intervention seems to be the key in recovering from Achilles tendonitis. I also encourage stretching to all my athletes. It is an easy thing to skip as it is time consuming and we can be pinched for time. Additionally, hydration is essential and I find collagen supplements to be beneficial as well. If you have any signs or symptoms do not delay. I can help get you back out participating in your favorite activities. If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Timothy Young Talks About Tight Calves and Foot Problems
Dr Timothy Young Talks About Tight Calves and Foot Problems
As mentioned, the mechanical load on the foot from the calf and ultimately the Achilles is tremendous. So, with equinus ( a tight calve and or Achilles) there are many problems. Think of a woman who wears high heel shoes every day for many years and over time the calf gets less flexible. Now with that tight calf, her gait has changed. As she walks, with each step going forward that tight calf pulls, and her heel comes off the ground early. Early heel off with gait leads to early transfer of weight and force to the front of the foot. Over time, this extra pressure on the front of the foot can cause problems. This is like the childhood toewalker, but with adult body size and weight.
If you are experiencing any foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr. Timothy Young Talks About Crossover Toe

This typically involves the second toe. This is where the second toe deviates toward the great toe and can even ride over the top of the great toe. When this happens, the structure back at the knuckle behind the toe itself (second MTP joint) becomes out of alignment and can be subluxed. In severe cases the joint can also dislocate. This causes a tremendous amount of stress on the 2nd MTP joint capsule. It's not uncommon for the capsule to become attenuated or stretched and thinned out. It can have partial tearing. This can lead to pain in the joint and inflammation with local swelling.
Dr. Brandon Nelson Discusses How To Stop Heel Pain And Plantar Fasciitis Once And For All

I’m still constantly surprised on a daily basis how many people live with chronic heel pain. Plantar fasciitis or heel pain can be so challenging for patients and really be detrimental to their life. I see a lot of patients that have suffered for years and years from heel pain and have seen multiple physicians and are still having pain. I empathize with these patients and understand their frustration as this can really impact their life and the things they want to do. Having suffered from plantar fasciitis and heel pain myself and knowing how it impacted my life, I really enjoyed treating heel pain patients.
I now important it is for me to maintain an active and healthy lifestyle and I really want to provide this for my patients as well. Often times the majority of heel pain gets treated as plantar fasciitis when there are quite a few other pathologies that can cause heel pain. I can’t stress enough compounded is to find the underlying causes of heel pain which allows proper treatment plan to occur. If you suffer from heel pain for plantar fasciitis and are continuing to suffer please make an appointment or give us a call today at 425-391-8666 today and we will help you stop it once and for all.
Dr. Brandon Nelson Discusses How To Resolve Heel Pain (Plantar Fasciitis) Without Physical Therapy

Heel pain or plantar fasciitis continues to be the number one reason people visit a foot and ankle doctor or a podiatrist. Heel pain or pain when you first get up in the morning can be extremely uncomfortable. Many patients that we treat have seen multiple other doctors or physical therapists. Patients have often spent months going to physical therapy and are continuing to go weekly.
I think physical therapy is a great modality and can be highly beneficial for many conditions. However, for heel pain or plantar fasciitis we almost never send patients to physical therapy. The reason being is we cure the problem. At Issaquah Foot & Ankle Specialist, home of the Washington Heel Pain Center we have developed a protocol that has an almost 100% cure rate for plantar fasciitis. If you are still suffering daily with heel pain come see us and we will help you get rid of it once and for all. Give us a call at 425-391-8666 or make an appointment online. Our Issaquah Podiatrists would love to see you!



