podiatrist issaquah
Displaying items by tag: podiatrist issaquah
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Why Toes Are Often Pinned During Foot Surgery
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Why Toes Are Often Pinned During Foot Surgery
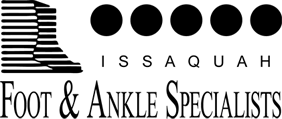
Pinning toes (with a K wire) is a common practice with foot surgery. In reality what is called a pin is a Kirschner wire or K wire. The K wire is typically is placed directly within the bones of the toe. The purpose is to hold the toe incorrect alignment. For example in other parts of the body including midfoot, ankle and leg when there's a fracture often a cast will work. But one can not effectively cast a toe. Therefore pinning a toe is an excellent option that holds it stable to allow for the correct healing and the correct alignment to be maintained during the postop time frame. For example, a patient with a hammertoe will have a contracture and adaptation of the proximal interphalangeal joint or the first knuckle within the toe.
This bone has to be surgically remodeled to allow for realignment. Once the bone remodeling is done, rather than just putting a bandage on the toe, a K wire is used in the toe to make certain that the correction and alignment are maintained exactly as necessary and so that the postoperative healing will continue in the correct alignment until that initial healing is adequate. In some cases the toe is actually fused and typically the K wire with stay in between four – six weeks. The closer to the six week timeframe, the higher correlation with long-term successful fusion.
If you are experiencing foot or ankle pain, please give us a call at 425-391-8666 or make an appointment online today.
Dr Brandon Nelson, A Board Certified Physician and Surgeon, Discusses Relief from Neuromas
I see many patients that come in for burning or tingling of the forefoot. Some even relate a stabbing or shooting pain in the front of the foot. Typically they often describe pain that is worse with shoe gear and relieved by taking off their shoes and rubbing their feet. These are very typical symptoms of somebody with nerve pain.
Neuromas are one of the most common causes of nerve pain in the feet, specifically the forefoot. Neuromas occur typically in females between the ages of 40-60, however they are common in men of the same ages as well. The neuromas itself occurs where two nerves in the feet come together. These two nerves are the medial and lateral plantar nerves that are branches of the posterior tibial nerve. They come together to form one nerve in the 3rd interspace of the foot. This is the region between the 3rd and 4th toes.
Most people will present with numbness and tingling. However some patients just present with pain to the toe or toes. Often there can be a change in shoe gear or activities that precipitate the nerve irritation. The prevailing theory is that this nerve is getting mechanically stimulated or crushed by the surrounding structures or the foot, most likely the metatarsal bones. Repetitive irritation leads to the symptoms that we see i.e., numbness and pain.
There are many great options to relieve nerve pain or neuroma pain. However the most important part of that is identification of the cause. It is paramount to see a provider that has experience and expertise in this area. I have been treating neuromas for over 15 years and have many excellent options to relieve pain and neuromas symptoms long term. If you are experiencing nerve pain I would love to help you get your life back. Give us a call at 425-491-8666 or make an appointment online.
Sincerely,
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Burning & Tingling in the Feet
Burning and tingling can be very uncomfortable for anybody, especially when it occurs in the feet. We often think of nerve issues when we hear this type of presentation from a patient. Stabbing, burning and tingling are all sensations that can be attributed to dysfunctional nerves. These types of symptoms can occur with rest or even after exercise. I encourage you to seek help earlier with nerve type pains.
The most common cause of nerve pain is diabetes. Diabetes can cause nerve sensitivity, a term referred to as neuropathy. Most patients with neuropathy, more specifically diabetic neuropathy usually have a long term history of elevated glucose levels. The neuropathy can present in both hands and feet.
Another common cause can be compression issues around nerves. Most people have heard of carpal tunnel, a nerve dysfunction that occurs in the wrist, well you can get the same scenario in the ankle or foot. This happens when soft tissue structures press on nerves and the nerves swell and become inflamed and the usual result is numbness or tingling.
Neuromas are another big cause of burning in the feet. These usually are more common in females and present with ball of foot burning. The most common area affected from a neuroma is the 3rd and 4th toes. Typically we see the pain is better without shoes and can increase with shoe pressure.
If you are suffering from numbness, tingling or burning I can help. Please call and schedule an evaluation today 425-391-8666 or make an appointment online.
Sincerely,
Dr Brandon Nelson
Dr. Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Heel Pain, Sore Heels and Heel Pain Treatment

Heel pain can have many causes and can be extremely challenging for all patients. Not all sore heels are caused by plantar fasciitis and it is important to understand the underlying cause. Identifying the underlying cause will help to assure patients get the best treatment options. Even with many other causes of a severe heel pain, the number one cause continues to be plantar fasciitis.
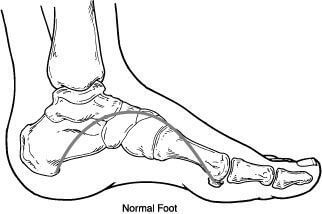
Plantar fasciitis is basically an inflammatory process of the main supporting network of the foot. The primary cause of inflammation seems to be overuse and repetitive stress. The plantar fascia in general has a relatively poor blood supply and this can lead to chronic inflammation. Once we see chronic inflammation set in it can become extremely difficult to reduce pain and resolve one's heel pain.
Heel pain treatment options are vast. It really boils down to what the primary cause of the heel pain was and the activity level of the patient. I like to break it down to foot structure and rear foot pathologies. What I mean by foot structure is does the patient have a high arched foot or a low arched foot. Is there a lot of pronation that occurs with ambulating or overloading of the foot? Rear foot pathology can have a large effect on heel pain. Is there a tight calf muscle or is there a dysfunctional supporting tendon? The best long term outcome and shortest course to a pain free heel is to appreciate the deforming forces.
If you have severe heel pain or pain under your heel or even pain with running I can help! Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr. Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Best Treatment Options for Hammer Toes
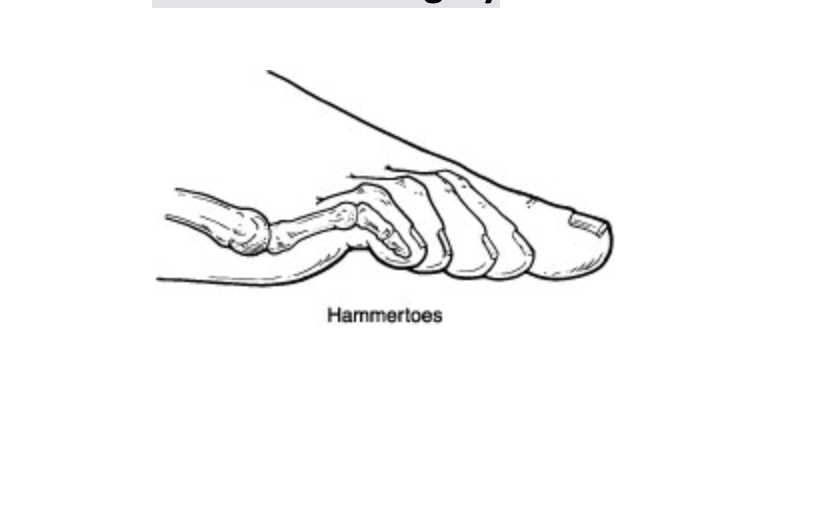
Hammer toes are quite common and can continue to get worse as time progresses. They are often associated with other foot deformities like bunions or flat feet but can be a standalone pathology. There is usually a family history associated with them or an underlying trauma that caused the development of the hammer toe or toes. Additionally, they can occur with over powering of certain tendons in the foot. The majority of hammer toes will require surgical care but some can be managed with padding and strapping.
Conservative care of hammer toes can be helpful especially during the initial development. There are several techniques for tapping hammer toes and even straps and splints that can be purchased to help control the toes. It is also advisable to stretch the calf and not go barefoot. However the vast majority of hammer toes will get worse and eventually require surgical intervention.
Surgical care for hammertoes can be divided into two types of procedures, soft tissue and bone. The determining factor for which procedure is appropriate is based on the clinical exam of the toe and the patient. Release of the long flexor tendon can be helpful in controlling the hammering digit as long as it is a flexible deformity. We often see this in the pediatric or geriatric patient as the hammer toes first develop. The longer the hammer toe is present the more likely bone work will need to be done. The most common procedure is a resection of the phalangeal head of the affected digit. Hammer toe surgery done in isolation allows for full ambulation after the procedure.
If you have hammer toes or other digital deformities I can help. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr. Timothy Young, a Board-Certified Foot Surgeon Discusses Porokeratosis Lesions
These lesions also can be in a non weightbearing portion of the foot such as the heel. These lesions can be challenging to treat. There is some preliminary data that the Swift treatment (Microwave Verrucae treatment) can help reduce the pain from these lesions and in some cases, there can be reduction or resolution of the lesions. Surgical excision of the porokeratosis lesions is another treatment option. Larger lesions can be surgically removed, and a plastic surgical technique called a rotational flap is utilized to repair the deficit left after removal of the larger lesions.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Plantar Verruca and Porokeratosis
Typically, this skin infection develops additional blood vessels through a process called angiogenesis. Therefore, it is classic for plantar verruca have multiple punctate or pinpoint patches of dried blood or eschar, and during the examination when we lightly remove the superficial layer of the verruca and callused area, we see pinpoint bleeding. This pinpoint bleeding is very helpful to accurately diagnose these as plantar verrucae. There is a similar appearing lesion that is often called a porokeratosis.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr. Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Neuroma Pain
Pain in the forefoot can range from tingling and burning to a dull ache or throb. The majority of forefoot pain can be broken down into nerve pain ie a neuroma or mechanical pain ie capsulitis. Both can cause similar type symptoms and differentiating between the two can be difficult.
Capsulitis is the most common forefoot type of pain. It is basically an overloading of the metatarsal phalangeal joints. Most patients will experience a combination of burning and aching. There are many causes of forefoot capsulitis or overloading. This can be from tight muscle groups or abnormal anatomy. The majority of patients will find conservative therapies successful and will completely recover.
Neuromas usually occur in a specific anatomical location, the 3rd interspace. This pain is almost exclusively a burning or tingling. It is almost always worse with shoes and primarily affects females. Neuromas occur from irritation to the nerve that is mechanical or anatomical in nature. Again the conservative success rate for this is high.
If you are experiencing burning or tingling in the foot I can help. I have an exceptional protocol for both capsulitis and neuritis. If you have foot pain, call today.
Sincerely,
Dr. Brandon Nelson, A Board Certified Physician & Surgeon, Discusses How To Get The Best Possible Bunion Surgery

Bunion surgery is one of the most common procedures performed in the United States. It is almost exclusively done in an outpatient setting and the majority of procedures can be completed in less than 2 hours. Most patients will experience pain that lasts a few days and can begin weight bearing fairly soon. There are many different types of bunion surgery and not all are equally effective.
There are a few things that will help patients get a better outcome with bunion surgery. I will discuss these tips that can be helpful along with selection of the surgeon.
#1. The most important thing after having any type of surgery is to follow postoperative protocol. There are many tips that can improve your outcome after bunion surgery and careful adherence to postoperative protocols is essential.
#2. Bone healing supplementation, there are many different types of bone healing supplementation that are not all created equal however some of them can be highly effective in decreasing healing times. I have a brand that I recommend for all my patients that often shaves weeks off of healing time.
#3. Couch potato for your first week, set yourself up for success. During that first week just really take it easy, take your medications as prescribed, ice and elevate your foot.
#4. Surgeon selection, the majority of us have very similar training and most foot and ankle physicians are highly trained in this procedure. One question I would ask any surgeon is how many bunion surgeries they perform annually.
I hope this is helpful and can be utilized by you in the future.
Sincerely,
Dr. Timothy Young Discusses Achilles Tendon Injuries
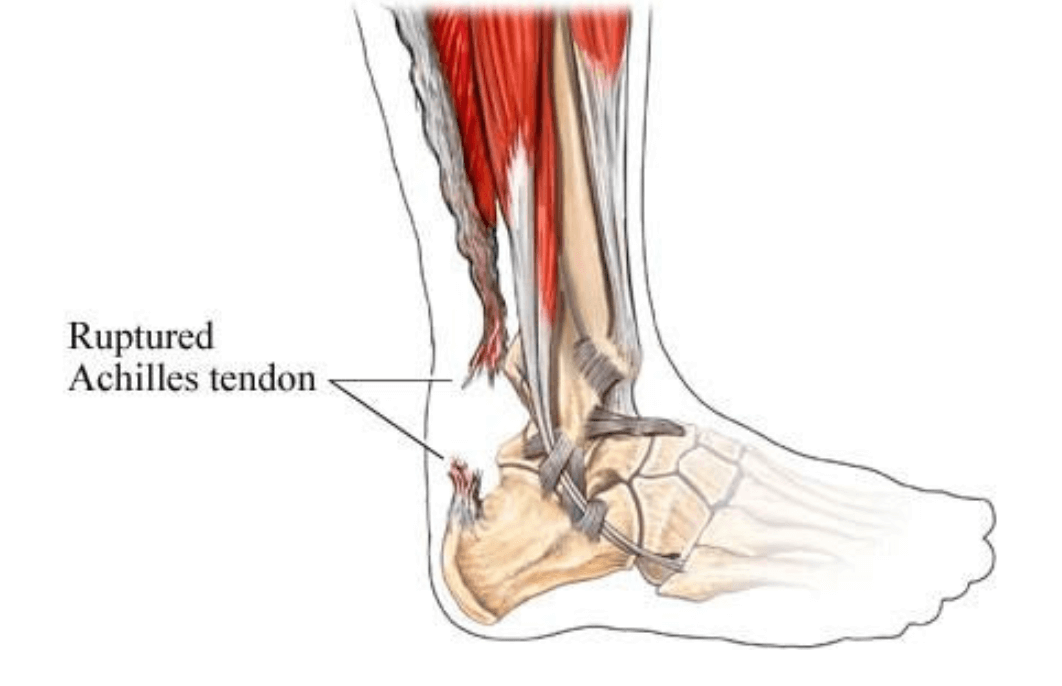
Dr. Timothy Young Discusses Achilles Tendon Injuries
Some of this can be done under the direction of the physical therapist. One of the most effective long-term exercises to augment any Achilles problem is eccentric Achilles strengthening. This also can be done at home or under the direction of the physical therapist. There are numerous YouTube videos on this including a short one that we have provided from our clinic.
Give us a call today at 425-391-8666 or make an appointment online for an evaluation.