podiatrist issaquah
Displaying items by tag: podiatrist issaquah
Dr Timoth Young, Board Certified Foot Surgeon talks about Lapidus and Lapiplasty Fixation: Advancements in Foot and Ankle Surgery
Dr Timoth Young, Board Certified Foot Surgeon talks about Lapidus and Lapiplasty Fixation: Advancements in Foot and Ankle Surgery Part 1
Introduction: Foot and ankle disorders can significantly impact a person's quality of life, affecting their ability to walk, stand, and perform daily activities. Over the years, surgical techniques and technologies have evolved to address these issues effectively. One of the notable advancements in foot and ankle surgery is the Lapidus and Lapiplasty fixation procedures. In this blog, we'll delve into what these procedures are, how they work, and their benefits for patients.
Lapidus Fixation: The Lapidus procedure, also known as the first tarsometatarsal (TMT) joint arthrodesis, is a surgical technique designed to correct deformities in the first metatarsal and medial cuneiform bones of the foot. This procedure is commonly used to treat conditions such as hallux valgus (bunions) and hypermobility of the first TMT joint. The primary goal of the Lapidus procedure is to achieve stability in the joint, alleviate pain, and improve the alignment of the foot.
During the Lapidus procedure, a surgeon makes an incision on the top of the foot near the first TMT joint. The joint is then realigned, and screws or other fixation devices are used to hold the bones in their corrected positions. Over time, the bones fuse together, creating a stable and properly aligned joint. This fusion eliminates the pain associated with joint movement and provides long-lasting relief.
Lapiplasty Fixation: The Lapiplasty procedure is a modern advancement in foot surgery that specifically targets bunions by addressing the root cause of the deformity. Unlike traditional bunion surgeries that focus on removing the bony bump, the Lapiplasty procedure aims to correct the misalignment of the metatarsal bone responsible for the bunion formation. This technique not only provides a more aesthetic result but also reduces the risk of bunion recurrence.
During the Lapiplasty procedure, a surgeon makes a precise cut in the metatarsal bone to realign it to its proper position. Specialized instrumentation is used to stabilize the bone, and fixation plates and screws are inserted to secure the corrected alignment. This approach allows patients to bear weight on the treated foot shortly after surgery, resulting in a faster recovery compared to traditional methods.
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Bunion Pain and How to Fix It
.jpg)
Bunions are often a painful condition especially when trying to fit certain shoes or exercise. Let us first discuss what a bunion is then how we can relieve the pain.
A bunion results from a combination of familial inheritance and environmental factors. Meaning that if you do not have a genetic predisposition for a bunion, you will not create one by adding outside forces to your foot. Where this becomes important for example is high heel shoes. If you have a family history of bunions and you wear high heels you can accelerate the process of development of the bunion. Or if you are an avid exerciser like a runner this can speed up the development of a bunion.
So what is a bunion? Well, there is a common misconception that a bunion is growth. This is not true nothing grows with a bunion it is from a misaligned bone in the foot. The culprit is the 1st metatarsal. This bone begins to shift out of place and cause a bulge on the inside of the foot and continues to get worse until the big toe has rotated. The bunion will get bigger as time goes on and often can begin to force the other toes out of position. Bunions at this point become painful and hard to fit in shoes.
What can be done for bunion pain? There are a lot of different things I can provide to relieve bunion pain. It really requires an evaluation of the bunion. But generally, wider shoes can help and prevent going barefoot. There are other options that provide more relief, but it really depends on the stage of the bunion.
If you are experiencing bunion pain I can help call to make an appointment with me at 425-391-8666 or fill out a contact form online.
Sincerely,Dr Brandon Nelson
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Bunion Surgery and How to Recover Faster

Bunion surgery is one of the most common procedures done in the United States. It is recommended most of these are done in an outpatient setting and patients can go home the same day. Most procedures are done in about 2 hrs and patients can walk in a protective boot. Most bunion procedures involve cutting bone or realigning joints.
Since bone is cut it is important to take calcium or a bone healing supplement. These can help decrease healing time and make recovery much easier. Additionally, I like my patients to use a bone stimulator and remain home for the first couple days. Sacrificing a little time on the front end of the surgery can make recovery much easier. Another supplement like collagen can help with skin healing and provide better scar appearance.
The vast majority of bunion surgeries can be done in our office. A mild anesthetic and a little bit of local anesthetic will provide enough comfort to sleep right through the procedure. Having it done in our office setting, in a sterile environment, provides large cost savings and time savings for patients.
If you have a bunion and are in pain, I can help. Make an appointment today with me at 425-391-8666 or contact us online.
Sincerely,
Dr Brandon Nelson
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses ForeFoot Pain or Pain In The Front Of One’s Foot
The front of your foot or the area where your toes begin is called the forefoot. This area consists of your toe bones, your phalanges and your metatarsals, the long foot bones. This area is where you push off when ambulating and provides stability for forward propulsion. This is a complex anatomical area and more than a few pathologies can exist in this location but I will discuss a few of the most common. These include neuromas, capsulitis and stress fractures.
Neuromas are an entrapped nerve that can cause burning and tingling. These usually occur in the 3rd interspace. Most patients have a sensation that is electrical and is worse in shoes and relieved by taking off their shoes and rubbing the forefoot. These seem to be more common in women than men and especially around the 4th-6th decade of life. Neuromas have some great treatment options available one of most successful is dehydrated alcohol injections. The success rate with these injections approaches 89%.
Capsulitis is a term we use to describe inflammation of a joint. This most commonly occurs in the metatarsophalangeal joint of the foot. We tend to see this in a patient with a bunion or high arched foot. The main cause seems to be a biomechanical imbalance. It is important to get an x-ray with capsulitis as arthritis can have a similar presentation.
Stress fractures usually present with swelling. They often occur as one begins a new training program and can cause pain for weeks. Typically these will be relieved with rest and exacerbated by activity. Most will heal with a change in activities and calcium supplementation. However again an x-ray is warranted to rule out other pathologies and to monitor healing.
If you are having forefoot pain I can help. Schedule an appointment with Dr Brandon Nelson, give us a call at 425-391-8666 or make an appointment online.
Sincerely,
Board Certified Physician & Surgeon
Dr. Timothy Young Discusses Bunion Surgeries Part 3
.jpg)
Dr. Timothy Young Discusses Bunion Surgeries Part 3
After the surgery Dr. Young likes to keep close tabs on his patients' and their recovery. It is important that any post procedure pain is well-controlled. It is also important that they have proper instructions beforehand, so they are prepared at home when all the anesthetic wears off. This is where being a couch potato pays off. Keeping the feet elevated, using ice, and taking medication as prescribed is critical. It is also critical to protect the surgical site either using a special boot, splint, crutches, or scooter. All the presurgical advice like getting a shower protector keeping the dressing intact to protect the surgical site comes into play. At each postoperative visit, the surgical site is checked to make certain it is healing properly and that there are no signs of infection.
Post acute recovery involves:
This involves bone remodeling and healing and soft tissue remodeling and healing. Sutures are removed. Post procedure x-rays are taken to verify the correction is maintained and that the bones are starting to bridge together properly. Our patients take special bone healing supplements also. We also often work with outside physical therapy clinics to help our patients heal faster and obtain proper range of motion and strength.
In conclusion, preparing for bunion surgery requires a comprehensive approach that considers the patient’s medical history, the extent of the deformity, and the type of surgery required. A skilled surgeon will carefully plan the surgery, provide detailed instructions for pre- and post-operative care, and closely monitor the patient’s recovery to ensure the best possible outcome.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr Timothy Young Discusses Bunion Surgeries

Dr Timothy Young Discusses Bunion Surgeries in Detail, Part 1
Bunion surgery is a common procedure performed by Dr Timothy Young and other Foot Surgeons to correct a bunion deformity. A bunion is usually combination of the first metatarsal being out of alignment and bony bump that forms on the joint at the base of the big toe. This can cause pain and discomfort when walking or wearing shoes. The bunion correction surgery itself usually takes 1-2 hours. The surgeon’s preparation for bunion surgery requires planning ahead and, requires attention to detail. In this blog, we will go over the steps that Dr. Young and other foot surgeons take to prepare for the best bunion treatment and the best bunion surgery.
Patient Evaluation
Before any bunion surgery, Dr. Young will evaluate the patient's medical history, medications, and overall health to make sure that our patients are good surgical candidates. Dr. Young will also examine the patient's foot to determine the severity of the bunion, the extent of the deformity, and the type of bunion surgery that would be most appropriate. For example, some patients have a severe bunion deformity and require a Lapidus or Lapiplasty procedure. Some patients have extreme adaptation of the great toe joint and require a procedure that realigns the joint. Some bunions are mild and yet the joint is not flexible and for this, decompressing the joint is an effective treatment. These evaluations come from both physically examining the foot, and imaging evaluation.
Imaging Tests
The surgeon will typically order imaging tests such as X-rays, CT scans, or MRI scans to get a better understanding of the bunion’s structure and position. This information will help the surgeon plan the surgery and determine the best approach to correcting the deformity. Dr. Young uses digital x-rays which allow for precise measurements and preoperative planning that can be done right on the computer.
Anesthesia Planning
Dr. Young will discuss the anesthesia options before surgery. Dr. Young often utilizes local anesthetic combined with MAC anesthesia (monitored anesthesia with conscious sedation). Other options include general anesthesia, regional anesthesia, or local anesthesia. The type of anesthesia can be discussed prior to surgery and will depend upon the patient's medical history and the type of foot surgery and the extent of bunion surgery. With MAC anesthesia combined with local anesthetic, the patient is still conscious and breathing on their own (not intubated). This is more like a twilight sleep and the patient's recovery extremely fast, and we can avoid the typical side effects that can be encountered with the general anesthetic.
The preoperative visit:
Dr. Young's patients come in the week prior to surgery to help them prepare for surgery. We will discuss details of the surgery itself and how to care for the foot after bunion surgery and if crutches or a special boot will be required. Also, the patient's medical history and medications are reviewed. Some medications will be avoided prior to surgery. Usually, the patient will be required to fast prior to surgery and need to make driving arrangements after the procedure. Our patients are given a special antibacterial scrub to do at home prior to surgery.
If you are experiencing foor or ankle pain, give us a call at 425-391-8666 or make an appointment online.
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Everything You Need To Know About Your Bunion

Bunions are primarily a genetic foot structure that is inherited from mom or dad. We see that it can skip generations as well. There seems to be a misconception that the bunion is just a growth on the side of the foot. However, this is not true. The bunion is a misalignment of the first metatarsal. It occurs when the first metatarsal separates or begins to deviate from the second metatarsal towards the other foot. This in turn causes the big toe to deviate or point towards the second digit. The growth or bump that one sees is the first metatarsal pointing out of the joint. This concept is important to understand as it will make sense when I discuss bunion correction.
Bunion correction refers to removal or reversal of the bunion. Well now that you understand it is a deviation, more correctly a progressive deviation of the first metatarsal, you can see why certain things will not correct a bunion. I have seen all sorts of strapping, taping and splinting techniques to correct a bunion. Now that it is clear this is a movement of a bone you can clearly see why none of this works. It is not possible to move the first metatarsal back into place once it has deviated via any sort of appliance or device you apply to the outside of the foot. Once the bone has moved the only option to correct the bunion is surgical.
Surgical correction of the bunion is the only way to reverse this misalignment. This is the only avenue we have to bring the big toe back into the correct orientation. There are many different techniques based on the size of the bunion and the rest of the foot structure. If you have a bunion and need help please schedule an appointment. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Achilles Tendonitis
Many athletes will suffer from the dreaded Achilles tendonitis. Increased training and often a change in activities can precipitate this pathology. It is quite frustrating and can sideline many active patients. I personally have dealt with this issue and can understand the challenges associated with it.
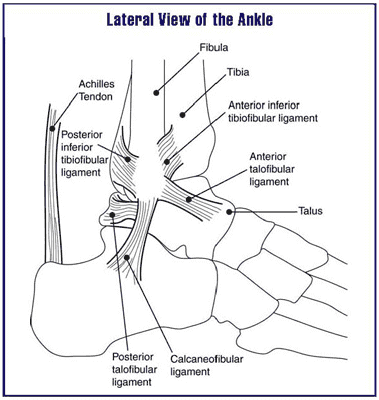
The Achilles tendon is the main unit in the lower extremity for the push off phase of gait. It contracts and helps individuals with forward motion. It is constantly under load and being utilized with every step. It is a wonder that more people don’t suffer from tendonitis.
The main cause continues to be overuse. It often is seen in runners and joggers and triathletes. In my office, runners seem to suffer from it. Runners seem to have the biggest demand on this tendon and overuse is quite easy. However, they are not the only one’s, basketball players seem to be affected as well. Probably related to the loading requirements of jumping. Regardless of the causes, it is important to seek help early in the process.
Early intervention seems to be the key in recovering from Achilles tendonitis. I also encourage stretching to all my athletes. It is an easy thing to skip as it is time consuming and we can be pinched for time. Additionally, hydration is essential and I find collagen supplements to be beneficial as well. If you have any signs or symptoms do not delay. I can help get you back out participating in your favorite activities. If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Healing From Bunion Surgery

There are many different types of bunion surgeries. The majority that are performed currently can be divided into two types. The first being a procedure at the head of the first metatarsal and the second at the base of the first metatarsal. The recovery and healing time frames vary according to which procedure a patient has.
Head procedures or an Austin type bunionectomy is the most common bunion surgery in the United States. I believe this represents something like 70% of all bunion surgeries. These procedures are much faster to heal and typically a patient can bear weight the entire postoperative course. The typical patient can be back in a shoe at about 6 weeks and return to full activities about 3 months.
Base procedures or a Lapidus type or Lapiplasty often requires longer to heal. Additionally there is variation among weight bearing with these cases. Some doctors will allow immediate weight bearing and some will require 6-8 weeks of non-weight bearing. Again, most people can return to activities about 3 months and into a normal shoe around this time as well.
Things that can improve bunion healing are diet, supplements and bone stimulators. From a dietary standpoint it is important to incorporate lots of green leafy vegetables during the postoperative phase. Supplements can play a role in healing as well. One of my favorites is called ProBono. This product provides all the minerals and nutrients for bone healing and helps to reduce time to heal. Bone stimulators can be applied to stimulate bone growth. These are harder to come by and often insurers will not approve these devices unless you have significant comorbidities. If you have a bunion and would like to have it fixed and have the least amount of down time I can help. Give us a call at 425-391-8666 or make an appointment online today.
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discuss Heel Pain

Heel pain can usually be broken down into a few main causes. The first and most common is plantar fasciitis. This is usually pain right at the bottom of the heel bone towards the inside arch. The second most common cause is Achilles tendonitis. This pain is more found towards the back of the heel. Lastly there is a condition called Baxter’s neuritis that can cause burning in the foot. This pain is usually on the inside of the foot.
Plantar fasciitis is by far the most common cause of heel pain. It is typically seen in adults between the ages of 40-60. Typical symptoms are pain in the morning or pain after rest. It is often an overuse type injury. Plantar fasciitis can usually be treated successfully and the protocol I use keeps people exercising for the duration of treatment.
Achilles tendonitis usually presents with swelling near its insertion towards the back of the heel. Sometimes a catching or popping can be felt. This is also another pathology associated with overuse. I cannot stress enough that this should be evaluated immediately.
Baxter’s neuritis is a little trickier. This condition usually presents as a burning in the heel but can mimic plantar fasciitis. I usually see this in conjunction with plantar fasciitis. This pathology usually requires special testing to identify.
If you have heel pain I can help. I think this is some of the most frustrating injuries to deal with especially for the people that are training. If you are experiencing heel pain, give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson



