podiatrist issaquah
Displaying items by tag: podiatrist issaquah
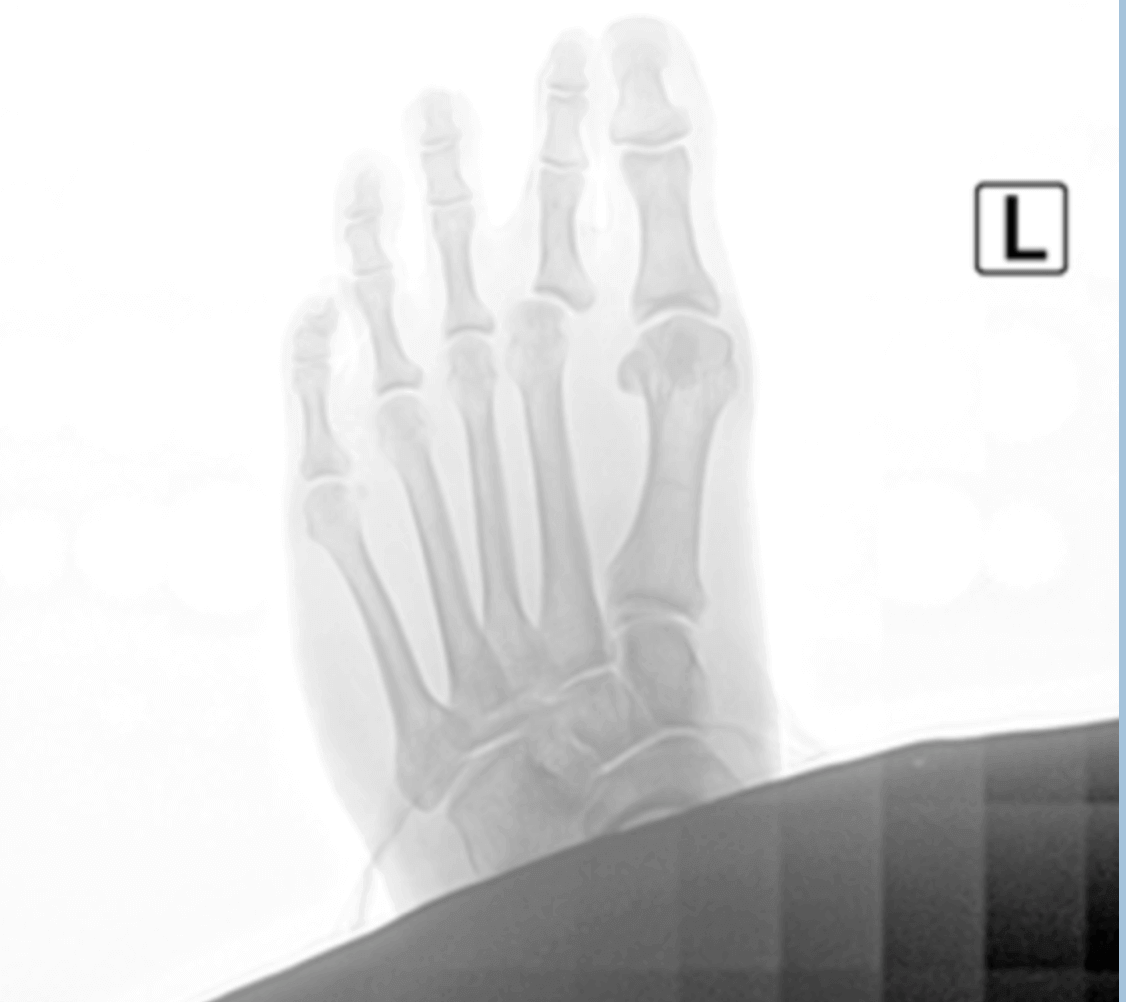
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses How To Make Sure You Have a Successful Bunion Surgery
.jpg)
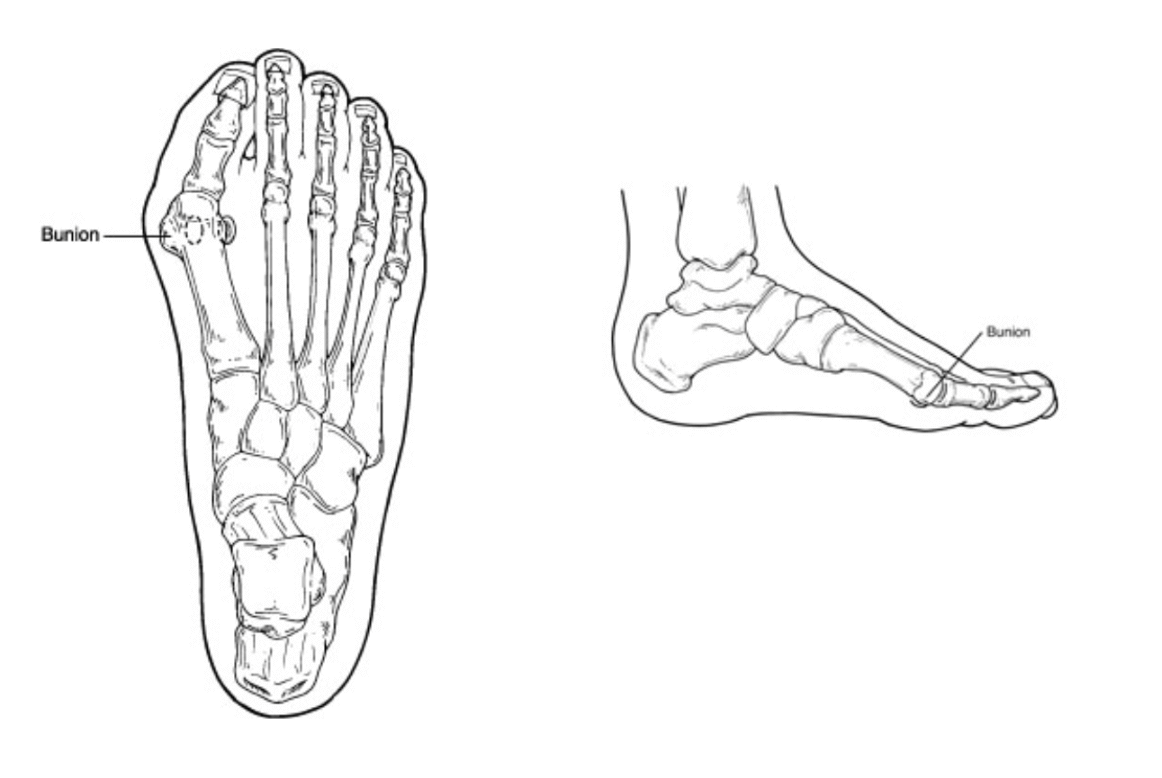
Bunion surgery is one of the most common surgeries performed in the United States. It is something like 250,000 operations annually, that is a lot of bunions! Well, how can you maximize your results, get back to activities early and heal faster? I will give you some insight on these questions.
Maximizing bunion results, when I think about what this question means I think it would pertain to how you get the best outcomes. This means to me how you make the foot more functional and get a good cosmetic result. This would be best done through appropriate procedure selection. There are a lot of different bunion operations that are used to fix different sizes of bunions and different foot structures. To me the most important thing here is to select a bunion surgeon that does a lot of bunions.
How do you get back to activities earlier? The main point here is to follow your surgeon's protocol. Do not listen to your neighbor or friend, they might have had a different operation than you. Your surgeon really knows best in this case. Most of us have taken years to perfect our post-op protocol and do not deviate from following them to the letter. But if you have questions or concerns ask to let us know.
Healing faster can mean a lot of things, the skin, the bone, when one can walk. The skin is the first thing to heal. I always recommend collagen and zinc supplements. These seem to speed things along and once the incision is closed there are some great products to minimize scar appearance. Next is the bone, a good bone healing supplement is essential and if available a bone stimulator can shave weeks off healing. Weight bearing is a different story, often this depends on other procedures that were done. I try to get all my patients moving and bearing weight within a couple days if appropriate. The minimum is to start a range of motion exercises.
If you would like a consultation on your bunion, I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Tips To Get Ready For Bunion Surgery
Bunion surgery is the most common surgical procedure I perform at my ambulatory surgery center. I have a few tips I would like to share that can make things much easier.
Get ready a week before surgery. Start thinking about where you will set up. I always recommend being a couch potato for about a week. This home base spot should be conveniently located. This spot should be downstairs and near a restroom. Make sure you have access to anything that might pass the time, a computer, tv, etc.
Meals are another thing to think about. I like to advise my patients to make a weeks’ worth of food. You can freeze them or refrigerate them but not having to cook can be a game changer. This can really help you focus on your recovery, and nobody wants to cook with a sore foot.
Supplements are another thing to consider. I think talking to your surgeon about this one is important. Calcium or some sort of bone healing supplement if you are having bone work done. Collagen and zinc can help wound healing. Once the wound closes, start topical scar care.
The bathroom situation can need some thought as well. How will you shower or use the toilet? I always if you are going to be non-weight bearing to have a trial run of both. It can be difficult executing these tasks with one foot. Options for these include a shower chair or stool and for the toilet they make elevated seats that are helpful.
Medications are the last thing I will touch on. Get these before the day of your procedure. Think about making a log or schedule so you can track what and when you take them. Make sure you understand what each is and that you have no interactions with other medications you are taking.
If you would like a consultation on your bunion, I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses The Benefits of Having The Lapiplasty Bunionectomy

I remember performing my first bunion surgery over 15 years ago and was so excited to help my patient. I also remember learning all the different types of bunion surgeries and how each one was slightly different. It made me ponder why there were so many different types of bunion surgeries for one pathology. It was about this time I was introduced to the Lapidus bunionectomy by an attending physician. He discussed how this was his favorite procedure, how it provided great outcomes but was difficult to execute.
Well fast forward 15 years and now the Lapidus is one of the most common bunion surgeries in the United States. Things have really changed with the Lapiplasty system. A group of doctors worked with a medical device company to develop a series of gigs and clamps to make the Lapidus reproducible and easier to perform. This has really revolutionized bunion surgery and I anticipate Lapidus will eventually be the most common surgery worldwide.
I feel lucky having trained in the Northwest as I am very familiar with the Lapidus procedure and even before the Lapiplasty system it was one of my go to bunion corrections.
If you have a bunion, you know how uncomfortable they can be. If you would like a consultation on your bunion I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Treatment Options for Hammer Toes
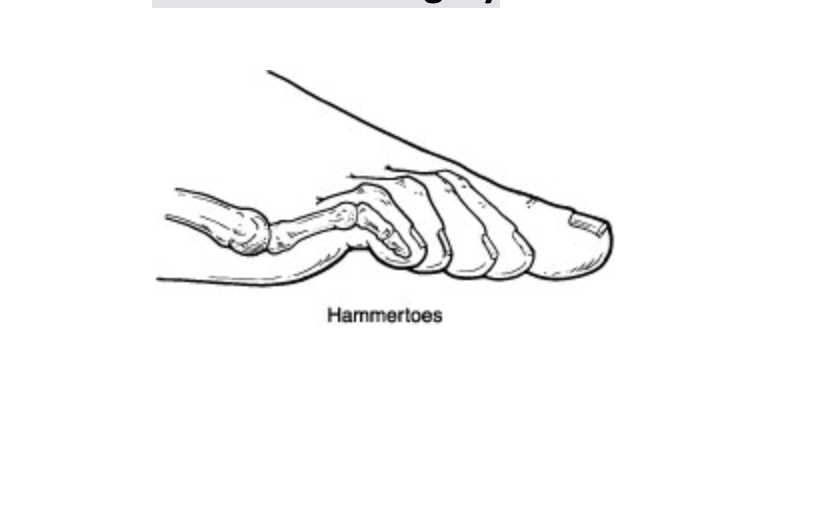
Hammer toes refer to a curling downward of the toes. This can occur in one or more toes and can be a stand-alone pathology or with another type of foot condition like a bunion. The hammer toe is often caused by shoe gear choices, trauma or inherited from mom and dad. It typically gets worse with time and makes it hard to exercise or fit in shoes properly.
The conservative options for hammer toes can sometimes relieve pain. These options are such things as wearing larger or wider shoes, taping the toes, or using pads or spacers. It is important to note that this does not fix the hammer toe. Additionally, with time it usually gets worse and the toe curls more.
Long term or surgical correction is the usuals course for most patients. This involves addressing the underlying causes of the hammertoe or toes. It is important to look at the overall foot structure and any contributing factors. The surgical procedure to correct a hammer toe can be removal of a bone or removal of a bone and soft tissue balancing. Sometimes it requires pinning of the hammer toe to allow the new position to heal and correct itself.
If you would like a consultation on your hammer toes I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr. Timothy Young, a Board Certified Foot Surgeon, Discusses My Top 5 Reasons Why I Recommend the Lapiplasty Bunion Repair
Dr. Timothy Young, a Board Certified Foot Surgeon, Discusses My Top 5 Reasons Why I Recommend the Lapiplasty Bunion Repair
Introduction
Bunions can be painful and disruptive, affecting the quality of life for many individuals. Traditional bunion surgery, also known as a bunionectomy, has been the standard approach for decades. However, in recent years, a groundbreaking surgical technique called Lapiplasty has emerged as a game-changer in the field of bunion repair. Surgeons worldwide are increasingly recommending Lapiplasty for several compelling reasons. In this blog, I will review the top 5 reasons why I recommend the Lapiplasty Procedure for bunion surgery.
1. Superior Three-Dimensional Correction
One of the most remarkable aspects of Lapiplasty is its ability to correct bunions in three dimensions, addressing the root cause of the deformity. Traditional bunion surgery often focuses on the visible bony bump, leaving the underlying bone misalignment uncorrected. Lapiplasty, on the other hand, repositions the metatarsal bone, restoring its proper alignment in all three planes—sagittal, transverse, and frontal. This three-dimensional correction not only provides better cosmetic results but also reduces the risk of bunion recurrence, making it a preferred choice among surgeons.
2. Faster Recovery and Reduced Downtime
Lapiplasty's minimally invasive approach and stable fixation results in faster recovery times for patients. Unlike traditional bunion surgery, which often requires patients to remain off their feet for an extended period, Lapiplasty allows patients to bear weight on their feet and start walking within days. This accelerated recovery can significantly improve a patient's overall experience and quality of life during the healing process.
3. Long-Lasting Results
Surgeons recommend Lapiplasty due to its track record of providing more durable and longer-lasting results. Traditional bunion surgery may offer temporary relief, but recurrence rates can be high. The Lapiplasty's comprehensive correction of the deformity decreases the likelihood of bunions returning, allowing patients to enjoy a more permanent solution to their foot pain.
4. Stable Fixation
The Lapiplasty utilizes very stable plates. These allow earlier weightbearing and return to activities. This fixation helps to promote optimal bone healing and long term stability. Surgeons who recommend Lapiplasty often highlight the fixation benefits of this innovative technique, which can boost patients' confidence and satisfaction with their results.
5. Evidence-Based Success
Surgeons have confidence in recommending Lapiplasty due to the strong evidence supporting its success. Numerous clinical studies and real-world cases have demonstrated the effectiveness of this procedure in addressing bunions, relieving pain, and improving patient outcomes. These data-driven results reassure both surgeons and patients that Lapiplasty is a reliable and proven treatment option.
Conclusion
Lapiplasty has revolutionized the field of bunion repair with its three-dimensional correction, quicker recovery times, long-lasting results, stable fixation, and evidence-based success. Surgeons worldwide recommend Lapiplasty as a superior alternative to traditional bunion surgery for patients seeking a more comprehensive and permanent solution to their foot pain. If you're considering bunion repair, please contact my office so I can evaluate your specific needs and discuss the benefits of Lapiplasty as a potential solution to your bunion woes.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Plantar Fasciitis Treatment Success with Shockwave Therapy

Plantar Fasciitis Treatment Success with Shockwave Therapy
Introduction
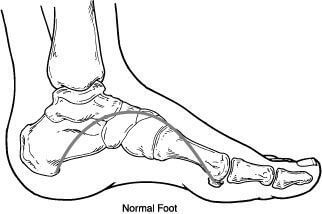
Plantar fasciitis is a common and often debilitating condition characterized by heel pain, especially in the morning or after prolonged periods of standing or walking. It occurs when the plantar fascia, a thick band of tissue that runs along the bottom of the foot, becomes inflamed or damaged. While there are several treatment options available, one that has gained increasing attention for its success is shockwave therapy. In this blog, we'll explore plantar fasciitis and delve into how shockwave therapy has emerged as a highly effective treatment option, offering hope and relief to those individuals suffering from this condition.
Understanding Plantar Fasciitis
Before reviewing shockwave therapy, it's essential to understand what plantar fasciitis is and why it can be so challenging to treat. The plantar fascia is a crucial component of the foot's structure, acting as a shock absorber and supporting the arch of the foot. When this tissue becomes damaged or inflamed, it can lead to persistent heel pain and reduced mobility.
Common Causes of Plantar Fasciitis:
Overuse or repetitive strain on the plantar fascia, often due to activities like running or standing for extended periods.
Obesity, as excess weight puts extra stress on the feet.
Improper footwear with inadequate arch support.
Tight calf muscles or Achilles tendon.
Traditional Treatment Approaches
Plantar fasciitis treatment typically begins with conservative methods, including:
Rest: Reducing activity levels to allow the plantar fascia to heal.
Ice: Applying ice to the affected area to reduce inflammation.
Stretching exercises: Focusing on calf stretches to improve flexibility.
Orthotics: Custom shoe inserts to provide arch and biomechanical support.
Non-steroidal anti-inflammatory drugs (NSAIDs): Medications to manage pain and inflammation.
While these methods can be effective for some individuals, others find themselves facing chronic, persistent pain that doesn't respond well to these treatments. This is where shockwave therapy comes into play.
Shockwave Therapy for Plantar Fasciitis
Shockwave therapy, also known as extracorporeal shockwave therapy (ESWT), is a non-invasive procedure that has shown remarkable success in treating plantar fasciitis when other treatments have failed. Here's how it works:
Application of Shockwaves: During the procedure, high-energy shockwaves are directed at the affected area. These shockwaves create microtrauma within the damaged tissue, stimulating the body's natural healing response.
Pain Reduction and Healing: Shockwave therapy has been shown to reduce pain by disrupting pain signals and improving blood flow to the damaged tissue. This, in turn, promotes tissue regeneration and healing.
Quick Procedure with Minimal Downtime: Shockwave therapy sessions typically last 15-20 minutes, and most patients can resume their regular activities shortly afterward. Five weekly sessions typically offer optimal results.
Success with Shockwave Therapy
The success of shockwave therapy in treating plantar fasciitis is supported by numerous patient testimonials and clinical studies. Here are a few reasons why it has gained popularity:
High Success Rate: Many patients experience significant pain reduction and improved mobility after undergoing shockwave therapy.
Non-Surgical: Shockwave therapy is non-invasive, eliminating the need for surgery and its associated risks and recovery time.
Long-Lasting Relief: For many, the benefits of shockwave therapy are long-lasting, providing relief from chronic pain.
Improved Quality of Life: Patients who have struggled with plantar fasciitis for years often find that shockwave therapy finally allows them to regain their quality of life and return to their favorite activities.
Available treatment: We have been proving this treatment at our clinic with high success for over 8 years
Conclusion
Plantar fasciitis can be a stubborn and painful condition, but there is hope for those who have tried various treatments without success. Shockwave therapy has emerged as an effective and non-invasive option, offering relief and improved quality of life for individuals suffering from this condition. If you're struggling with plantar fasciitis, please contact our clinic at 425-391-8666 or make an appointment online.
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Heel Pain That Will Not Get Better

I have had heel pain in the past, specifically plantar fasciitis and it really was challenging to go about your day. My pain when I got out of bed was uncomfortable until it loosened up but if I sat down for any period of time it came right back. Does this sound familiar? If it does and this pain just will not go away, I can help.
Plantar fasciitis is by far the leading cause of heel pain. The plantar fascia is a tough soft tissue structure that provides the most structural support to your foot. It works to prevent your foot from flattening out and helps control your foot for the gait cycle. It is vital for foot function and is under chronic tension. These factors make it one of the most common causes of foot pain.
Treating plantar fasciitis can often be difficult as well. There are many people that have seen a physician and still have been or have been working on their pain at home. I encourage you if this is you to see a physician that specializes in heel pain. I have been working with heel pain patients for over 15 years. I have seen every type of pain and can help cure even the most stubborn cases. If you want to get your life back and live without heel pain I can help, call to make an appointment with me at 425-391-8666.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Why You Should Have the Lapiplasty Procedure to Fix Your Bunion

Bunion surgery has been around for more than 100 years. It is one of the most common surgeries performed in the United States. Over 100,000 are done annually and the majority are on women. In recent years new advancements have been made to speed recovery and success of the operation.
The Lapiplasty system by Treace Medical is at the forefront of bunion repair. This system has taken years to develop and has undergone evolution as it has been utilized. It has now proven to be one of the work horses of bunion surgery. It provides reproducible results and long-term correction. It has an ease of use that makes the surgical procedure faster and improves recovery. This has changed bunion surgery for patients and surgeons. The Lapiplasty system is based on a long-standing surgical technique.
This long-standing technique was first described around the turn of the century by Paul Lapidus. He advocated that the bunion started from the tarsometatarsal joint, and correction needed to occur there. Since his original thought we have only worked to improve and support this theory in the surgical community. It has been shown this is the center of most bunions and the correction is best done here. If you have a bunion the time has never been better to have it fixed.
Lapiplasty is by far the most successful bunion surgery technique I have seen. If you are experiencing bunion pain, I can help call to make an appointment with me at 425-391-8666.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Things You Need To Know About Bunion Surgery

Surgery in general can be an overwhelming endeavor. There are often a lot of new instructions, medications, and appointments to keep track of. I have a few recommendations that can be helpful for anybody undergoing bunion surgery.
One of the first things to do is make a list. I love it when my patients show up with a list of questions at their pre-op appointment. This helps to make sure all topics are covered, and nothing is a mystery come surgery day. In that list often is a shopping list is helpful things like bandages, supplements, otc medications and healthy foods.
Getting a base of operation set up before surgery can help with easing the recovery. I recommend a place on the 1st floor if you have multiple levels. Somewhere that is close to the bathroom and is relatively quiet to aid in recovery. Ideally you have room for your post-op supplies nearby. It is also nice to have something in the room to help pass the time like a TV or music.
Personal hygiene is another area to touch on. I find it helpful for my patients to have some sort of stool to sit on in the shower. This helps reduce pressure on the operated foot. Additionally, if you are non-weight, bearing a toilet seat can be helpful. Practice, practice, and practice have some dry runs of showering and using the toilet before surgery to see if you need any other items. I think it is trickier than most of us remember to be off one foot.
Lastly a few miscellaneous tips;
1. Couch potato for the first 72 hours.
2. Elevating makes a big difference in long term swelling.
3. Take any recommended supplements.
4. Do not change the dressings unless instructed.
5. Lots of fluids.
6. Take a stool softener.
I hope these were helpful. If you are experiencing bunion pain, I can help call to make an appointment with me at 425-391-8666 or contact us online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Timoth Young, Board Certified Foot Surgeon talks about Lapidus and Lapiplasty Fixation: Advancements in Foot and Ankle Surgery Part 2
Dr Timoth Young, Board Certified Foot Surgeon talks about Lapidus and Lapiplasty Fixation: Advancements in Foot and Ankle Surgery Part 2
Benefits of Lapidus and Lapiplasty Fixation:
Improved Alignment: Both procedures aim to correct the alignment of the foot bones, which not only relieves pain but also helps restore normal foot function.
Faster Recovery: Lapidus and Lapiplasty procedures enable patients to return to weight-bearing activities sooner than traditional methods, reducing downtime.
Reduced Risk of Recurrence: Lapiplasty fixation, in particular, targets the underlying cause of bunions, reducing the likelihood of recurrence.
Long-Term Results: The fusion achieved through these fixation methods creates stable and lasting joint alignment, offering enduring relief from pain and discomfort.
Minimal Soft Tissue Disruption: These procedures typically involve less disruption of soft tissues, leading to reduced scarring and a potentially smoother recovery process.
Conclusion: Lapidus and Lapiplasty fixation procedures are innovative approaches to correcting foot and ankle deformities, especially bunions. With their focus on achieving proper bone alignment and stability, these procedures offer patients improved quality of life, reduced pain, and faster recovery times. If you're experiencing foot and ankle issues, consult a qualified orthopedic surgeon to determine whether Lapidus or Lapiplasty fixation could be the right solution for you. Always remember that personalized medical advice is crucial before making any decisions regarding surgical interventions.
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.



