bfdadmin
bfdadmin
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Plantar Verruca and Porokeratosis
Typically, this skin infection develops additional blood vessels through a process called angiogenesis. Therefore, it is classic for plantar verruca have multiple punctate or pinpoint patches of dried blood or eschar, and during the examination when we lightly remove the superficial layer of the verruca and callused area, we see pinpoint bleeding. This pinpoint bleeding is very helpful to accurately diagnose these as plantar verrucae. There is a similar appearing lesion that is often called a porokeratosis.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr. Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Bunions in Children

I see quite a few pediatric patients and a number of juvenile bunions. The major factor to development of a juvenile bunion is family history or genetics. Almost every child I see with a bunion has a family history of bunions. Usually mom and/or grandma have a bunion and often even their siblings have one. When bunions present early in development they can be difficult to manage. It is hard to find success in the conservative realm with bunions and quite a few require surgery.
Surgery for the juvenile bunion can be very rewarding and provide excellent long term results. First and foremost, it requires a physician work up and x-ray. Often there can be an underlying flatfoot with a juvenile bunion and not addressing this can lead to increased rate of recurrence. After a thorough history and physical the appropriate procedure can be selected. Typically a juvenile bunion will be fixed with a Lapidus type procedure.
The Lapidus or Lapiplasty is a highly successful procedure and has great long term outcomes. This involves a rotation correction of the bunion and a reduction in the splaying of the forefoot. There are many ways to fixate this type of correction for bunions and is surgeon dependent. It is amazing how quickly children heal from a procedure like this! If you have a child with a bunion and would like to have a consultation please make an appointment today. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr. Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Heel Pain That Will Not Go Away

The most common cause of heel pain continues to be plantar fasciitis. This is usually caused by a foot structure that puts too much pressure on the fascia or tight muscle groups. The majority of plantar fasciitis will go away with physician care and patients will return to normal activities. However, there are a few patients that their heel pain does not get better and need additional treatment.
If you are one of these patients it is important to see a physician that specializes in heel pain. There can be a few diagnoses that need to be considered for anyone that has recalcitrant heel pain. These can range from nerve to bone issues and a careful work up is warranted. Our practice has been home to the Washington Heel Pain Center for years. We were actually the first heel pain center in Washington State and then saw many other offices try to follow suit. However, our physician group finds heel pain fascinating and we diligently scour the latest research to remain up to date on causes and treatment options.
If you suffer from heel pain and have seen other doctors we can help. Or maybe heel pain is new for you and you want the best care we can help. We provide the best care and have the quickest options to get you back exercising or keep you exercising. Make an appointment today and we can help. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr. Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Neuroma Pain
Pain in the forefoot can range from tingling and burning to a dull ache or throb. The majority of forefoot pain can be broken down into nerve pain ie a neuroma or mechanical pain ie capsulitis. Both can cause similar type symptoms and differentiating between the two can be difficult.
Capsulitis is the most common forefoot type of pain. It is basically an overloading of the metatarsal phalangeal joints. Most patients will experience a combination of burning and aching. There are many causes of forefoot capsulitis or overloading. This can be from tight muscle groups or abnormal anatomy. The majority of patients will find conservative therapies successful and will completely recover.
Neuromas usually occur in a specific anatomical location, the 3rd interspace. This pain is almost exclusively a burning or tingling. It is almost always worse with shoes and primarily affects females. Neuromas occur from irritation to the nerve that is mechanical or anatomical in nature. Again the conservative success rate for this is high.
If you are experiencing burning or tingling in the foot I can help. I have an exceptional protocol for both capsulitis and neuritis. If you have foot pain, call today.
Sincerely,
Dr. Brandon Nelson, A Board Certified Physician & Surgeon, Discusses How To Get The Best Possible Bunion Surgery

Bunion surgery is one of the most common procedures performed in the United States. It is almost exclusively done in an outpatient setting and the majority of procedures can be completed in less than 2 hours. Most patients will experience pain that lasts a few days and can begin weight bearing fairly soon. There are many different types of bunion surgery and not all are equally effective.
There are a few things that will help patients get a better outcome with bunion surgery. I will discuss these tips that can be helpful along with selection of the surgeon.
#1. The most important thing after having any type of surgery is to follow postoperative protocol. There are many tips that can improve your outcome after bunion surgery and careful adherence to postoperative protocols is essential.
#2. Bone healing supplementation, there are many different types of bone healing supplementation that are not all created equal however some of them can be highly effective in decreasing healing times. I have a brand that I recommend for all my patients that often shaves weeks off of healing time.
#3. Couch potato for your first week, set yourself up for success. During that first week just really take it easy, take your medications as prescribed, ice and elevate your foot.
#4. Surgeon selection, the majority of us have very similar training and most foot and ankle physicians are highly trained in this procedure. One question I would ask any surgeon is how many bunion surgeries they perform annually.
I hope this is helpful and can be utilized by you in the future.
Sincerely,
Dr. Timothy Young Discusses Achilles Tendon Injuries
Dr. Timothy Young Discusses Achilles Tendon Injuries
Some of this can be done under the direction of the physical therapist. One of the most effective long-term exercises to augment any Achilles problem is eccentric Achilles strengthening. This also can be done at home or under the direction of the physical therapist. There are numerous YouTube videos on this including a short one that we have provided from our clinic.
Give us a call today at 425-391-8666 or make an appointment online for an evaluation.
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Morning Heel Pain

Heel pain can be very challenging no matter when it occurs. It can be common in the morning or after exercise. There are many causes of heel pain and the most common is plantar fasciitis. Plantar Fasciitis is a condition in which the plantar fascia in your foot becomes inflamed.
An inflamed plantar fascia is often characterized by burning or a bruised type sensation one's heel. Many patients describe the fact they feel like they are walking on a marble or pebble. This can get worse as time and activity levels go on and can become quite debilitating. This can be brought on by many causes but most notable is overuse.
Overuse is by far the most common cause. Patients often relate the start of a new exercise program or a new activity. This new activity can put new stresses on your fascia which ultimately leads to inflammation and pain. It is always best to ease into activities as this can help minimize fascial pain. Another key characteristic of facial pain is morning stiffness or irritation.
Morning pain is a hallmark of fasciitis. This is very common and one of the most challenging parts of having plantar fasciitis. This is often because when you sleep and then step down on your foot your fascia instantly becomes irritated. This can be extremely difficult to get rid of and often sticks around for months. This is when it is time to make an appointment with a heel pain specialist. I have been treating heel pain for 15 years and can help you get rid of it quickly. Give us a call today at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson
Dr. Timothy Young Discusses Achilles Tendon Injuries and Rupture - Part 2
Dr. Timothy Young Discusses Achilles Tendon Injuries and Rupture- Part 2
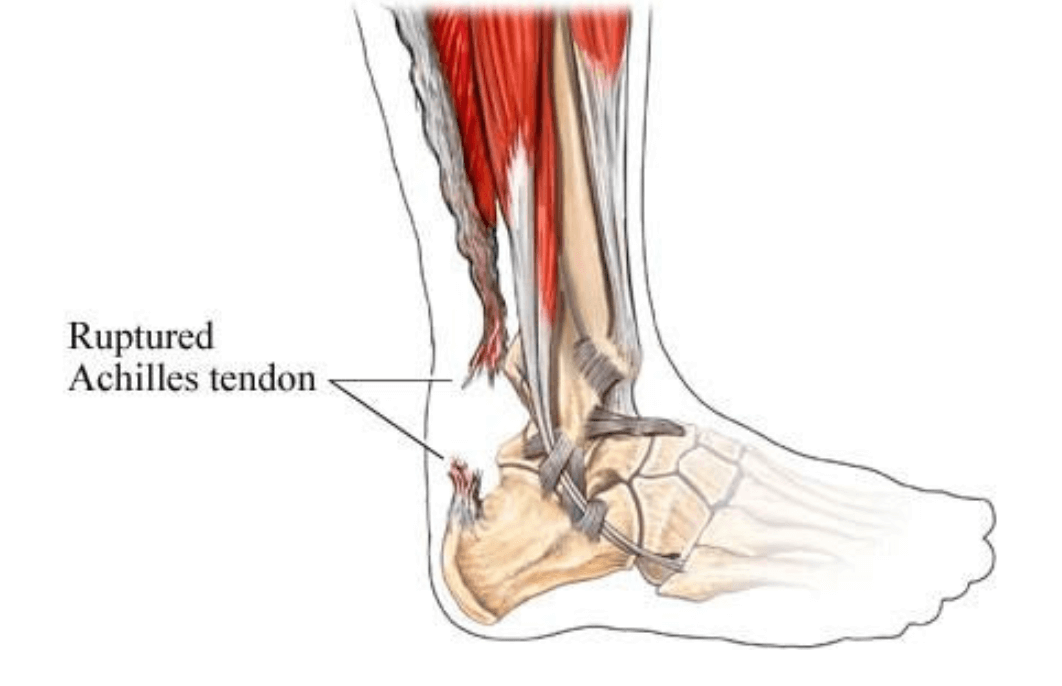
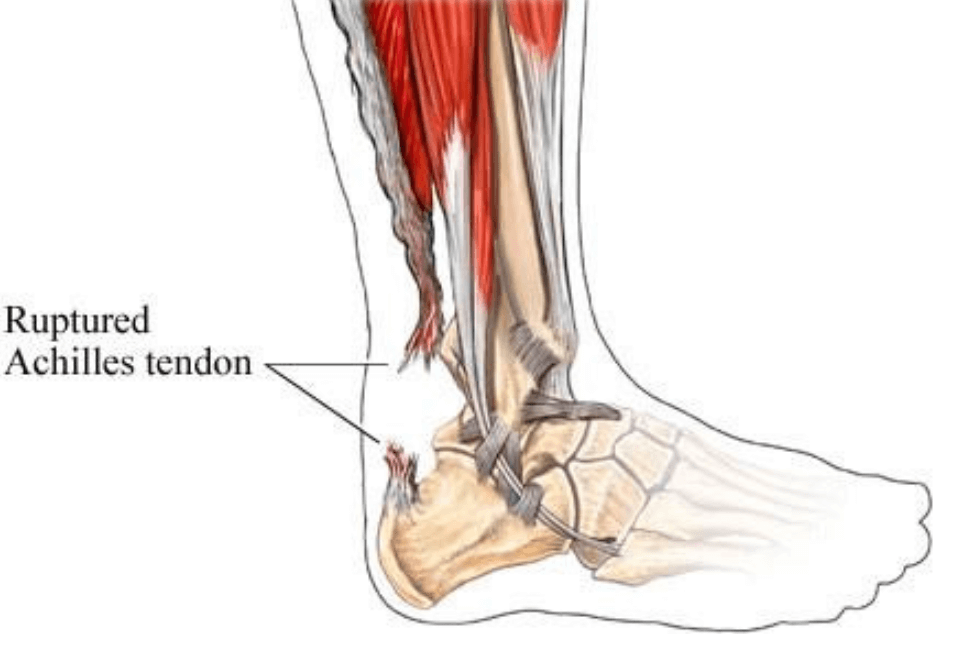
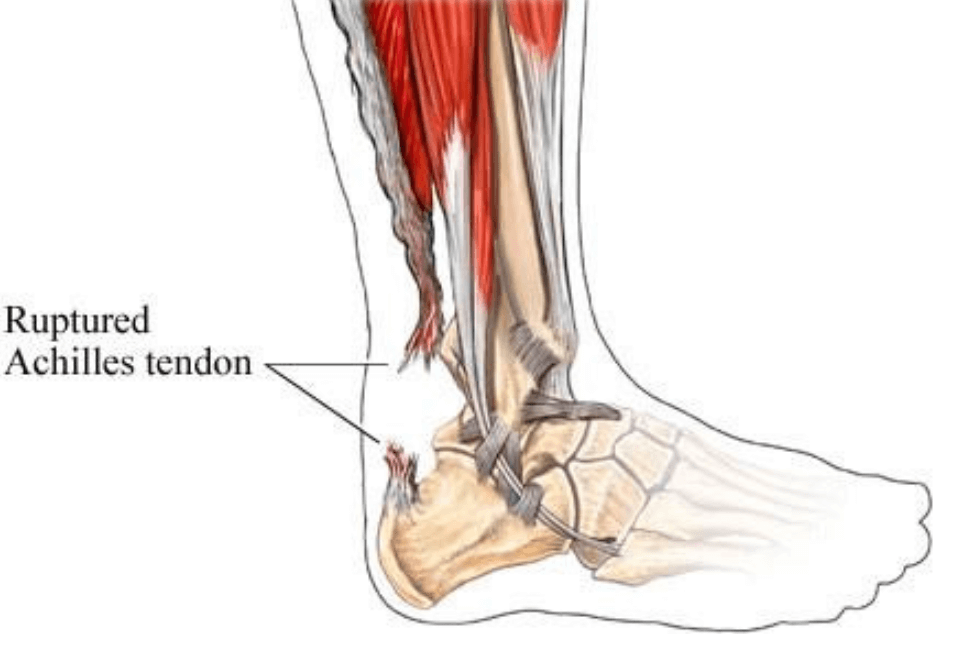
For those individuals that elect not to have surgical repair for an Achilles rupture, there will be a significant clot surrounding the damage portion of the Achilles tendon. This does serve a function and will help serve as a substrate that can later become scar tissue that helps augment the body's own Achilles repair. Because this is present from the original injury, additional treatment may be less beneficial for these individuals then with an open surgical repair.
After approximately three weeks post injury I would then recommend augmenting the Achilles injury with shockwave therapy (EPAT). The shockwave therapy is done at once per week, for total of five treatments. I always recommend supplemental collagen when there has been tendon damage and especially tendon rupture, whether open surgical repair or nonsurgical repair.
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr. Timothy Young Discusses Achilles Tendon Injuries and Rupture - Part 1
Dr. Timothy Young Discusses Achilles Tendon Injuries and Rupture
Part 1
We see a number of Achilles injuries in our clinic. For most active individuals with a complete rupture the Achilles tendon we advocate surgical repair. During the surgical repair any of the significant internal bleeding or hematoma is removed to facilitate the repair itself. After the repair has been done during the surgery we often augment this with other treatment. The original injury blood clot itself does have components that may be beneficial but some of those components also can become excessive scar tissue. Eventual augmentation with shockwave therapy can also benefit these patients who have had open surgical repair of an Achilles rupture.
If you are experiencing any foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr. Timothy Young, a Board-Certified Foot and Ankle Surgeon, Discuss His Treatment For Anterior Tibial Tendinitis
Whenever possible addressing the underlying mechanics is helpful. Also decreasing the activity that exacerbates is the problem and cross training is helpful. For example when playing tennis one might have to switch from singles to doubles and be aware of abrupt and sudden movements that will cause the foot to hit the ground quickly and with runners this may involve avoiding running hills and doing flat work instead.



