bfdadmin
bfdadmin
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Children's Foot Problems
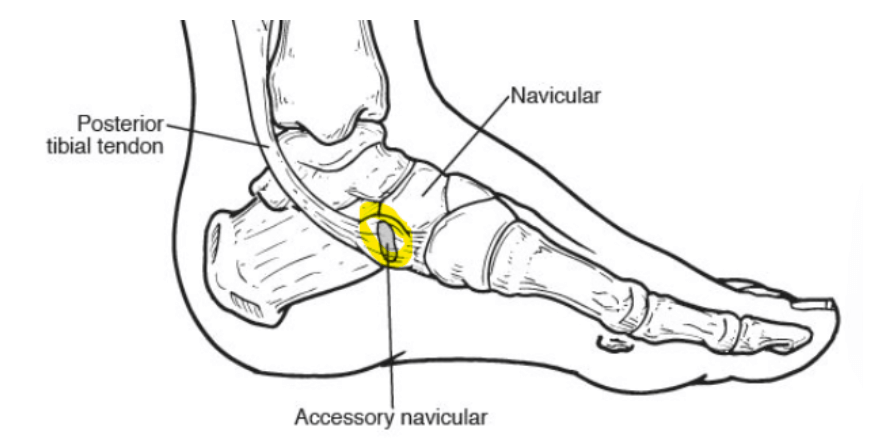
This attachment point can be overstressed with a pronated low arch foot structure. Basically the tendon has to work too hard and there can be pain and inflammation with the tendon attaches to the navicular. In other cases the tendon attaches to the accessory navicular bone which then attaches to the main navicular bone. This weakens the attachment point and creates more potential problems. In some cases, the accessory navicular has to be removed. This foot surgery procedure is called a Kidner procedure and is done at approximate 13 years of age with a range of 9 to 16 years of age for children. This is sometimes done in adults also. When the accessory bone is removed and the tendon is repaired it often improves the mechanical function of the tendon at this point. It also eliminates the inflamed and symptomatic accessory bone. The accessory navicular very common and is present in approximately 5-10% of the population. For milder cases, ankle braces orthotics and athletic taping can all offer some symptomatic and functional improvement with the painful accessory navicular.
If you or your children are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, Board-Certified Foot Surgeon, Discusses Painful Bumps and Bones That Stick Out on Children's Feet

Dr. Timothy Young, Board-Certified Foot Surgeon, Discusses Painful Bumps and Bones That Stick Out on Children's Feet
Up to 10% of the population may have this. Also the navicular bone itself even without the extra or accessory bone may be quite prominent. This is much more of a problem in children that have low arches/hyperpronation or flat feet. The posterior tibial tendon that attaches this location is at a strong mechanical disadvantage. On the outside or lateral aspect of the foot there may be a tailors bunion or bunionnette. And a smaller percentage of the pediatric population will have a growth plate or and apophysis of the 5th metatarsal base. This is called Iselin's disease. We will go over each of these more detail in some of our following blogs and discussion.
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online today.
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Finds the Lapiplasty Surgical Procedure for Bunions to be Highly Successful

I have been operating on bunions now for over 15 years and have seen all sizes and shapes of bunions. It is interesting to see the techniques that have come in and out of favor. I have had an opportunity to watch as the Lapiplasty has moved to the forefront of surgical procedures for bunion correction. I believe this is a great option for bunion repair and am excited to see what the future holds in regard to the Lapiplasty.
I find the Lapiplasy highly successful for large bunions or patients with flatfeet. The Lapiplasty provides great correction and faster recovery. It is an easily reproducible procedure with gigs and guides to help with correction. It provides for stable fixation and allows for early weight bearing. It can be used at all ages and helps to maintain long term correction. The system is revolutionary for surgeons and has taken years to develop.
I can say I am excited to continue using this system and to help my patients with bunions. It is wonderful to have a tool set like the Lapiplasty at my surgery center and to help so many patients walk normally again. If you have been contemplating bunion correction I would love to share this exciting new technology with you. Give us a call today at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Founder of the Washington Heel Pain Center
When I created the Washington Heel Pain Center I was excited to bring my years of treating heel pain to patients. I had seen and even experienced heel pain from all types of pathology and was ready to provide the best possible care for heel pain. Heel pain continues to be the most common reason for a patient to visit our clinic and we still provide the best care in Washington, Issaquah, Bellevue and Seattle. There are even offices now that have tried to imitate our heel pain center.
However, being the first heel pain center in Washington and the longest running heel pain center in Washington we continue to provide the best possible care. We have the most advanced technology to diagnose and cure heel pain. Our center provides the latest treatment options available to get patients pain free quickly and back to their favorite activities. Patients come to us from all over the Northwest including Alaska, Canada, Oregon and Idaho.
If you suffer from heel pain I can help. I see the average patient improve their symptoms by 50-70% in a week with my protocol. If you are in pain with every step or have pain when getting out of bed or after rest I can help. If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online today.
Sincerely,
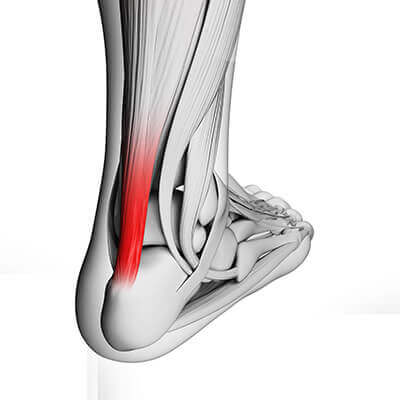
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Insertional Achilles Tendon Problems
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Insertional Achilles Tendon Problems
Especially very large areas of calcification with men. Although women can get a condition that similar but different called a Haglund deformity. In this case it is the bone on the posterior aspect of the calcaneus that protrudes and can be aggravated by the adjacent Achilles tendon and not intratendon calcification. In the early stages this is very treatable. As time goes on and there are large areas of calcification, they can cause chronic problems. As I mentioned, in the early stages this response to some of the classic treatments for Achilles problems. That means a special brace, orthotics to decrease the workload and side to side mechanical shearing of the tendon at the insertion point, calf stretching and related treatments, and shockwave therapy. The later stages the same treatments are often still helpful, but they may not offer full relief. These are the individuals that often require surgery. The surgery involves access to the back of the Achilles insertion point with removal of the calcific portions and then reattachment of the tendon itself. The healing process for this can be similar to an Achilles rupture. There are new anchors that help to give more reliable surgical reattachment of the Achilles to the underlying bone.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, a Board-Certified Foot Surgeon Discusses Tendinosis
The most effective treatments for this include prescription orthotics to address the mechanics and to reduce the mechanical shearing within the tendon. Calf stretching and a night splint can be very effective. KT tape is a useful adjunct for this problem. Shockwave therapy is extremely helpful for this condition. Some individuals will require surgery for this. This can involve removing some of the damaged portion of the tendon, and it can also involve lengthening the tight calf muscle with the gastrocnemius recession.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, a Board-Certified Foot Surgeon Discusses Achilles Tendon Problems
Dr. Timothy Young, a Board-Certified Foot Surgeon Discusses Achilles Tendon Problems
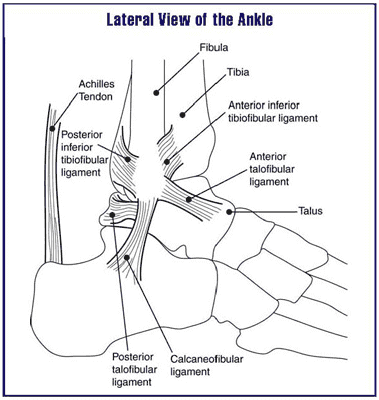
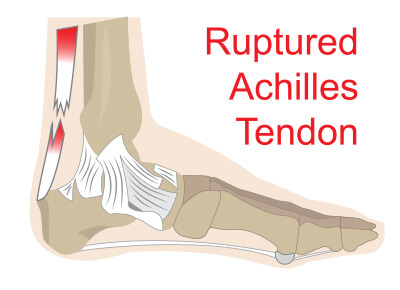
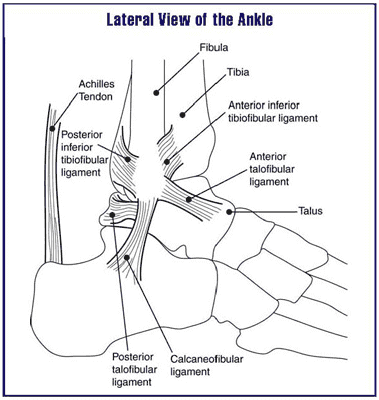
Achilles tendon problems can be quite different from other tendon conditions or pathology. There can be an acute inflammation or an acute strain, or there may be a chronic condition. Sometimes there is a low-grade condition smoldering along that the individual is not aware of and finally it passes a threshold of involvement that creates symptoms and pain. There is the main central portion of the Achilles tendon which is considered the watershed region of the tendon primarily because there is not as much blood supply to this area.
Then there is the outer synovial sheath adjacent to the tendon or the paratendon. There is no typical tendon sheath with the Achilles tendon but rather a paratenon which is a lining around the tendon. This can become inflamed. This would be considered paratendinitis or paratendinosis. And finally, there is the insertion of the tendon that can become degenerative and calcified. In addition, there can be a partial tear of the tendon or a total rupture. Therefore, there can be different approaches to treatment based upon which problem is encountered with the Achilles tendon.
There may be different causes of the specific condition which can help to dictate which treatments to focus on. In general, addressing a tight calf muscle is appropriate whether it is stretching the use of a night splint or even a gastroc recession or lengthening. Other general treatments include home physical therapy, prescription orthotics and addressing biomechanics, KT tape and icing, shockwave therapy. For some individuals' surgical treatment is appropriate.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, a Board-Certified Foot Surgeon Discusses Common Tendon Problems
Dr. Timothy Young, a Board-Certified Foot Surgeon Discusses Common Tendon Problems
Many of our patients have heard of tendon problems such as tendinitis. Over the last few years there has been some clarification of some of these tendon pathologies and conditions.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr. Brandon Nelson, A Board Certified Physician and Surgeon, Discuss When To Consider Having Your Bunion Fixed

The bunion deformity is an inherited foot structure issue. Most people that develop a bunion have a family history of bunions. They usually have a parent or grandparent that has a similar type of foot or foot problem. The foot structure that predisposes one to a bunion can be inherited. Usually this type of foot is more prone to flattening or pronating and this over time can result in a bunion. There are other factors that can accelerate the development of a bunion as well.
Wearing high heel shoes has been shown to put more pressure on the forefoot and therefore speed up the process of developing a bunion. Additionally any exercise that puts increased force on the foot can technically speed up the growth of a bunion i.e. running, jumping or similar exercises. The bunion develops as the body tries to stabilize the foot with these activities.
The bunion is a shifting of the 1st metatarsal bone to try and control abnormal flattening of the arch. This is one of the first adaptations the body utilizes. Patients often think there is a growth of bone at the site but technically it is the bone shifting out of place that occurs and creates the illusion of something growing. This is why there are no conservative measures that can move the bone back into correct alignment and why surgery is the only long term fix.
Surgery for bunion surgeries has really changed in the last couple decades. New techniques allow for a much faster recovery and healing times. If you have a painful bunion or would just like a consultation on bunions in general I can help. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,Dr Brandon Nelson
Dr. Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Heel Pain When You First Get Out of Bed

Waking up in the morning is hard enough. It becomes even harder when you have pain with putting your feet down. Morning pain or first step pain is usually an indicator of plantar fasciitis. I am going to briefly describe why we get it and what we can do to relieve it.
When we sleep at night our foot and ankle are in a plantar flexed position. This means our foot is bending forwards as well as our ankle. Positioning like this creates soft tissue relaxation. Specifically our Achilles tendon and plantar fascia have decreased tension on them. This allows tightening of our tissues and as we sleep the inflammation from the previous day settles in. Then as we place our foot on the ground to step out of bed we stretch and place load on the plantar fascia and the Achilles tendon. This causes pain and discomfort immediately and leads to a cycle of inflammation. There are a few tricks you can do to help this.
Morning pain can be alleviated and here are a few ideas to help;
1. Before you get out of bed, write the alphabet with your toes. This will help loosen up your tissue and stimulate blood supply and lubrication of those tendons and fascia.
2. Stretch, start with stretching in bed work on your posterior chain. It can be quite helpful to stretch your Achilles and your fascia.
I do think it is important to seek a physician before starting any of these options. It is essential to get a proper diagnosis and treatment plan. If you are having heel pain I can help. If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Sincerely,