bfdadmin
bfdadmin
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Heel Pain That Will Not Go Away

Heel pain is by far the most common thing I see in the office. The number one cause is still being plantar fasciitis. Most patients with heel pain will have resolution of their pain within a month of seeing me. However, there is a small percentage of patients that do not get better and further work up is warranted. We call these patients the outliers or red herrings. There are about 2 main causes of outliers or red herrings. These are nerve issues, i.e., Baxter’s neuritis or a stress fracture.
Baxter’s neuritis is not as common as plantar fasciitis. It is basically an entrapment of a nerve near the heel. The nerve becomes irritated and compressed. The symptoms can be similar to plantar fasciitis. The most common symptom seems to be burning in the heel. Burning or tingling are often associated with nerve pain. Usually, a nerve conduction study is required to diagnose this entrapment. Once it is diagnosed sometimes a local injection of the nerve can help or a prescription orthotic to offload the area can be quite helpful. Baxter’s neuritis differs from a stress fracture in presentation usually.
A stress fracture of the heel bone or calcaneus both can cause heel pain however usually in different areas. With the stress fracture it is usually a constant pain that is a dull ache or throb. Additionally, there is often an increase in training that has resulted in a stress fracture. Usually, a stress fracture will require an MRI and most resolve with time and protected weight bearing. If you are suffering from heel pain, especially if it has been going on for more than a couple weeks I can help. If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online.
Sincerely,
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses the Best Time to Have Bunion Surgery


Bunion surgery can be highly rewarding for patients. When you have a bunion that causes pain daily or pressure in the shoe it is a great time to think about having it fixed. Having a bunion fixed these days is easy and it is done in an outpatient setting.
Timing for some patients is critical. Many patients want to plan around a certain time of year or holiday. I personally believe that timing plays a big role and when it is easier in one’s life is a great idea. What I mean is we can all be busy and certain times of the year are less busy. Or for some certain times or the year are more important to patients. If you are a big skier and winter sports are important, do it in the summer or vice versa. Timing can be crucial but planning I feel is just as important.
Planning can also be extremely important. I recommend thinking about being a couch potato for the 1st week and making sure you are prepared for that. I think it is best to have food prepared, a place set up downstairs if that is appropriate, basically a command center you can live and work in. A place with a bathroom nearby and any way you can minimize having to get up and move around. Recovery is probably the next item we should talk about after planning.
Recovery varies by procedure and what other procedures were done. It can be as quick as walking in a normal shoe in 6 weeks or more like 19 weeks. Some procedures you will need to be on crutches as needed for pain others you may need them for 6 weeks. One could be running around 3 months but others it may be longer. It is important to be patient and allow adequate healing to occur and know it can often take up to 1 year. If you are suffering from heel pain, especially if it has been going on for more than a couple weeks I can help. If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online.
Sincerely,
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Conservative Care For Your Bunion

I get a lot of questions about what measures are helpful for conservative care of bunions. I think it is important to know that although there are no conservative measures that will ever reverse, fix or change the size or appearance of your bunion there are a few things you can do to help slow the progression of it. The only effective measure to ever fix or remove your bunion is surgical. There are a few things you can do to make your bunion more comfortable.
The first thing I always recommend is stretching your calf muscles. Your calf muscles impart force on your feet and lengthening them can help reduce this force. Google a couple calf stretching exercises and perform them a few times a day.
Secondly, no bare feet can be helpful. Most people that develop a bunion have a mechanically unstable foot. Wearing a sandal or slipper around the house can help slow the deforming forces creating the bunion. I like a good recovery sandal or a nice pair of slippers with arch support. Socks do not count, they do nothing to support your foot.
A prescription orthotic is your biggest help in slowing down the progression of your bunion. We are not talking about something you buy online, buy from a shoe store or some other venue. A prescription orthotic is made by a physician. This is a medical device that is often covered by insurance. This is made after a biomechanical examination of the lower extremity and gait. This is often done with a 3-D image of the foot to capture the foot structure.
Things that absolutely do not work and are a waste of money. Toe correction devices you see online. If a bunion could be fixed this way, there would never be another bunion surgery ever. Toe spacers can be helpful in reducing rubbing but again these will not fix your bunion. If you are suffering from bunion pain I can help. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Everything You Need To Know About Your Bunion

Bunions are primarily a genetic foot structure that is inherited from mom or dad. We see that it can skip generations as well. There seems to be a misconception that the bunion is just a growth on the side of the foot. However, this is not true. The bunion is a misalignment of the first metatarsal. It occurs when the first metatarsal separates or begins to deviate from the second metatarsal towards the other foot. This in turn causes the big toe to deviate or point towards the second digit. The growth or bump that one sees is the first metatarsal pointing out of the joint. This concept is important to understand as it will make sense when I discuss bunion correction.
Bunion correction refers to removal or reversal of the bunion. Well now that you understand it is a deviation, more correctly a progressive deviation of the first metatarsal, you can see why certain things will not correct a bunion. I have seen all sorts of strapping, taping and splinting techniques to correct a bunion. Now that it is clear this is a movement of a bone you can clearly see why none of this works. It is not possible to move the first metatarsal back into place once it has deviated via any sort of appliance or device you apply to the outside of the foot. Once the bone has moved the only option to correct the bunion is surgical.
Surgical correction of the bunion is the only way to reverse this misalignment. This is the only avenue we have to bring the big toe back into the correct orientation. There are many different techniques based on the size of the bunion and the rest of the foot structure. If you have a bunion and need help please schedule an appointment. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses How to Heal Quickly Following Bunion Surgery

There are a few things patients can do to heal faster from bunion surgery. I will review some ideas that patients can utilize that may decrease healing time frames. Most importantly one must follow the postoperative course as directed by your surgeon. It is important to realize that 2 things need to heal following surgery: soft tissues and bone.
Soft tissues consist of skin, subcutaneous tissues and capsular tissue around the joint. These structures are primarily sutured closed and will typically have sutures in for 10-14 days depending on the site. There are a few supplements that can help to improve healing. I like to have my patients take collagen and zinc and hydrate as these can influence skin healing. Once the wound is closed I encourage the use of silicone and moisturization of the wound. Additionally it is important to start the range of motion of the toe to free up and adhesions.
Bone is the other structure that must heal after bunion surgery. Usually, a bone cut, or fusion is performed. This is dependent on the procedure but there are a few things you can do to speed bone healing. The first being additional calcium and other bone healing nutrients. I like to have my patients take a bone healing supplement and increase the consumption of green leafy vegetables. Additionally, if a bone stimulator is available this can be helpful.
Regardless of the bunion procedure these tips can be helpful in your recovery process. Take care and wish you a speedy recovery. If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online.
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Achilles Tendonitis
Many athletes will suffer from the dreaded Achilles tendonitis. Increased training and often a change in activities can precipitate this pathology. It is quite frustrating and can sideline many active patients. I personally have dealt with this issue and can understand the challenges associated with it.
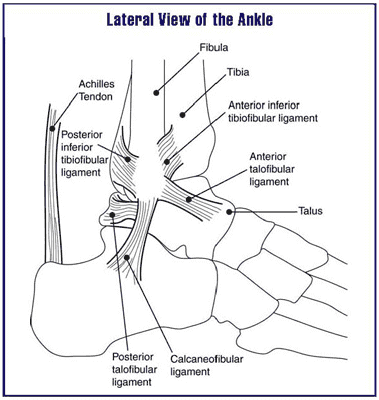
The Achilles tendon is the main unit in the lower extremity for the push off phase of gait. It contracts and helps individuals with forward motion. It is constantly under load and being utilized with every step. It is a wonder that more people don’t suffer from tendonitis.
The main cause continues to be overuse. It often is seen in runners and joggers and triathletes. In my office, runners seem to suffer from it. Runners seem to have the biggest demand on this tendon and overuse is quite easy. However, they are not the only one’s, basketball players seem to be affected as well. Probably related to the loading requirements of jumping. Regardless of the causes, it is important to seek help early in the process.
Early intervention seems to be the key in recovering from Achilles tendonitis. I also encourage stretching to all my athletes. It is an easy thing to skip as it is time consuming and we can be pinched for time. Additionally, hydration is essential and I find collagen supplements to be beneficial as well. If you have any signs or symptoms do not delay. I can help get you back out participating in your favorite activities. If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Healing From Bunion Surgery

There are many different types of bunion surgeries. The majority that are performed currently can be divided into two types. The first being a procedure at the head of the first metatarsal and the second at the base of the first metatarsal. The recovery and healing time frames vary according to which procedure a patient has.
Head procedures or an Austin type bunionectomy is the most common bunion surgery in the United States. I believe this represents something like 70% of all bunion surgeries. These procedures are much faster to heal and typically a patient can bear weight the entire postoperative course. The typical patient can be back in a shoe at about 6 weeks and return to full activities about 3 months.
Base procedures or a Lapidus type or Lapiplasty often requires longer to heal. Additionally there is variation among weight bearing with these cases. Some doctors will allow immediate weight bearing and some will require 6-8 weeks of non-weight bearing. Again, most people can return to activities about 3 months and into a normal shoe around this time as well.
Things that can improve bunion healing are diet, supplements and bone stimulators. From a dietary standpoint it is important to incorporate lots of green leafy vegetables during the postoperative phase. Supplements can play a role in healing as well. One of my favorites is called ProBono. This product provides all the minerals and nutrients for bone healing and helps to reduce time to heal. Bone stimulators can be applied to stimulate bone growth. These are harder to come by and often insurers will not approve these devices unless you have significant comorbidities. If you have a bunion and would like to have it fixed and have the least amount of down time I can help. Give us a call at 425-391-8666 or make an appointment online today.
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses How to Get Rid of Neuroma Pain Without Surgery
Neuromas are a benign proliferation of a nerve in the forefoot. There are many different theories on why this happens. Most doctors believe it is a compression of the nerve that causes the pain. The pain is often described as a sharp shooting electrical type of pain. This usually occurs between the 3rd and 4th digits in the foot. Neuromas are more common in women than men and usually occur between the 4 and 6th decade of life.
Neuromas treatments can vary from injections to wider shoes to surgical resection of the nerve. One of the most effective techniques for resolving neuroma pain is alcohol injections. This is where a physician injects dehydrated alcohol that helps to deaden the covering around the nerve. I have been utilizing this type of therapy for over 15 years. It continues to be the most effective treatment for neuromas I have seen. The success rate is close to 90%. This is a great option for long term relief of neuroma pain
Patients that fail alcohol injection therapy usually require surgical resection of the nerve. This involves a small incision on the top or bottom of the foot and dissection to the nerve which is then removed. This nerve that is removed is a sensory nerve so there is no loss of function but usually a small patch of numbness.
If you have been suffering from neuroma pain make an appointment today and I can help. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discuss Heel Pain

Heel pain can usually be broken down into a few main causes. The first and most common is plantar fasciitis. This is usually pain right at the bottom of the heel bone towards the inside arch. The second most common cause is Achilles tendonitis. This pain is more found towards the back of the heel. Lastly there is a condition called Baxter’s neuritis that can cause burning in the foot. This pain is usually on the inside of the foot.
Plantar fasciitis is by far the most common cause of heel pain. It is typically seen in adults between the ages of 40-60. Typical symptoms are pain in the morning or pain after rest. It is often an overuse type injury. Plantar fasciitis can usually be treated successfully and the protocol I use keeps people exercising for the duration of treatment.
Achilles tendonitis usually presents with swelling near its insertion towards the back of the heel. Sometimes a catching or popping can be felt. This is also another pathology associated with overuse. I cannot stress enough that this should be evaluated immediately.
Baxter’s neuritis is a little trickier. This condition usually presents as a burning in the heel but can mimic plantar fasciitis. I usually see this in conjunction with plantar fasciitis. This pathology usually requires special testing to identify.
If you have heel pain I can help. I think this is some of the most frustrating injuries to deal with especially for the people that are training. If you are experiencing heel pain, give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Finally Getting Your Bunion Fixed!

In the average week I see quite a few patients that are ready to finally have their bunion fixed. The large majority of patients I have seen for years and their bunions are becoming bigger and more painful. They are having a hard time fitting in shoes and going about daily activities. The decision to fix their bunion is an exciting one and today's repairs of a bunion are much easier than in the past.
Fixing your bunion is a big decision and it can be overwhelming sometimes. I really enjoy helping my patients through this process and eliminating the concern and apprehension around surgical correction. Surgery for bunions has really come a long way and new techniques have created an almost foolproof approach.
The newest technique that I am really excited about is the Lapiplasty. This is a great procedure that is reliable and has great long term results. The Lapiplasty is excellent for patients that even have large bunions. This procedure can be done in my office at our on-site surgery center. This can provide huge time and cost savings.
Do you have a bunion and have you always thought about fixing it? Give me a call and I can help. I look forward to fixing your bunion!!!! Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,



