bfdadmin
bfdadmin
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Why You Should Have The Lapiplasty Bunionectomy Procedure

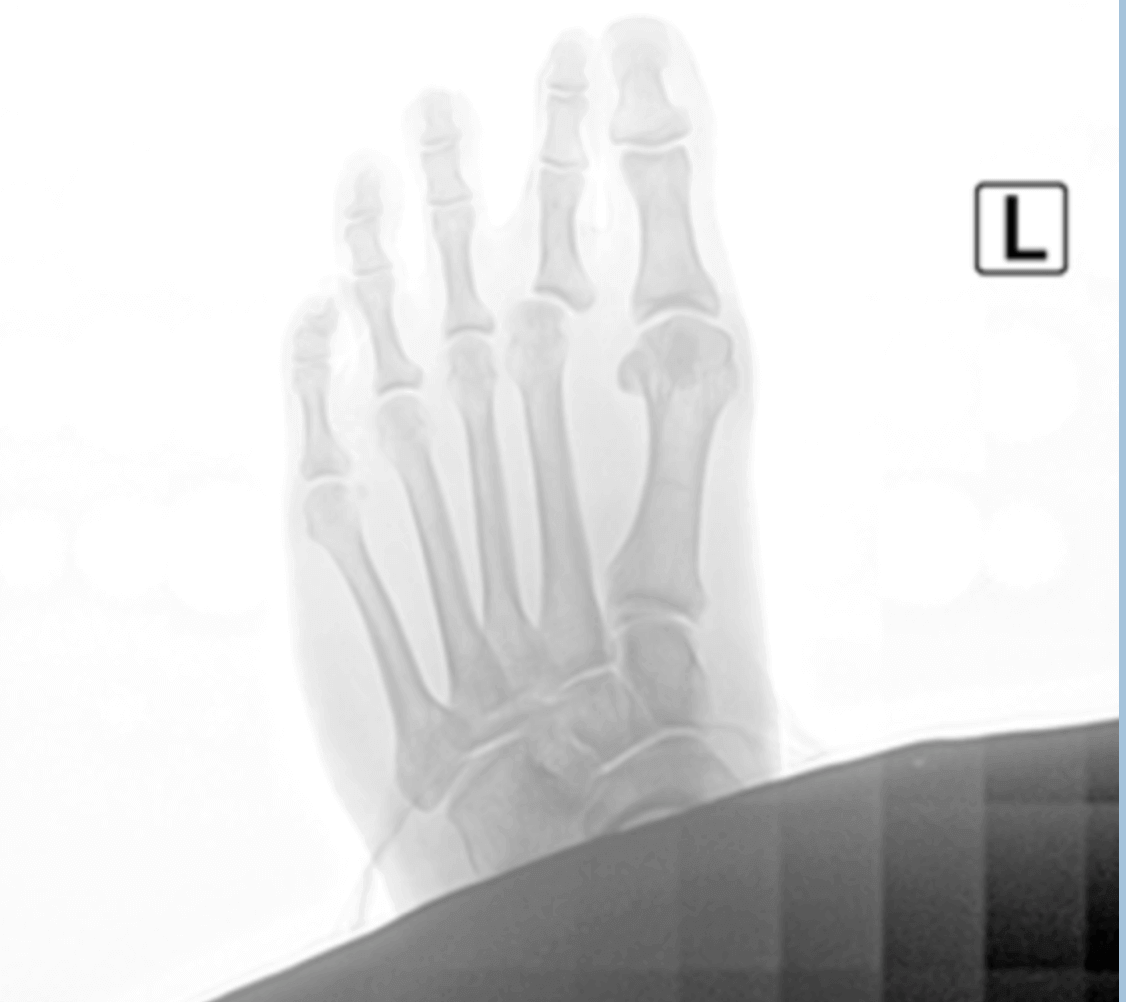
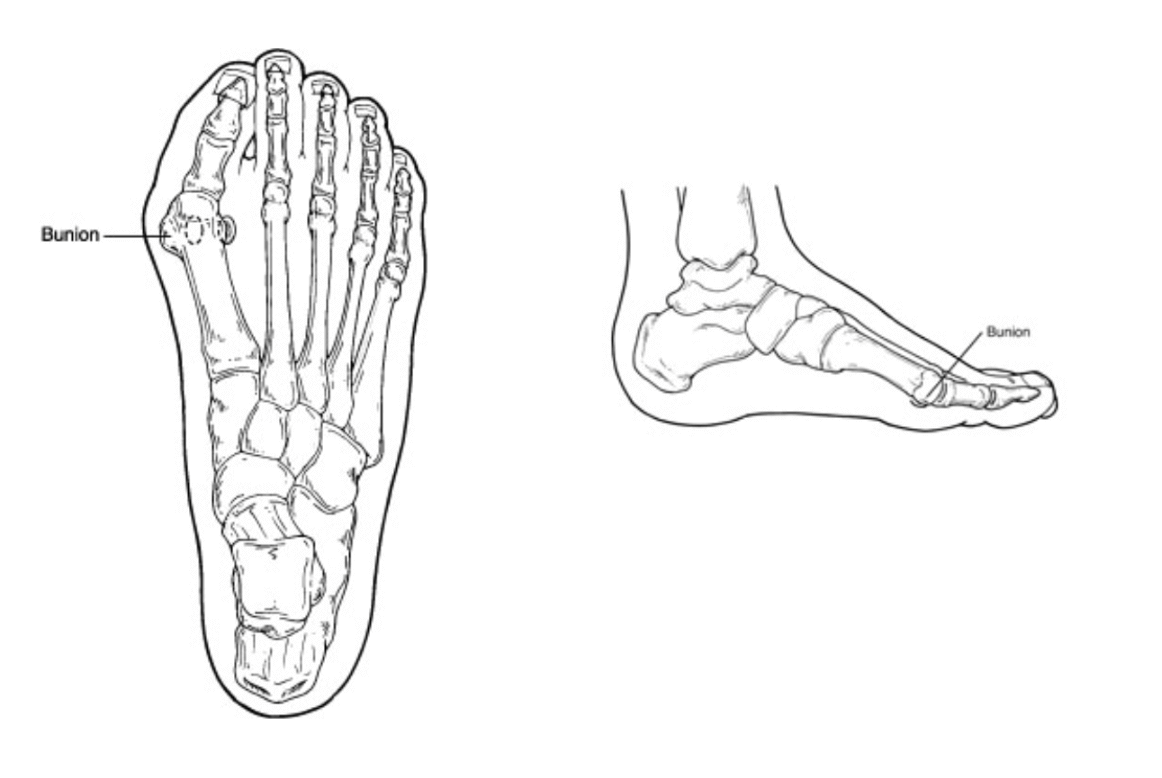
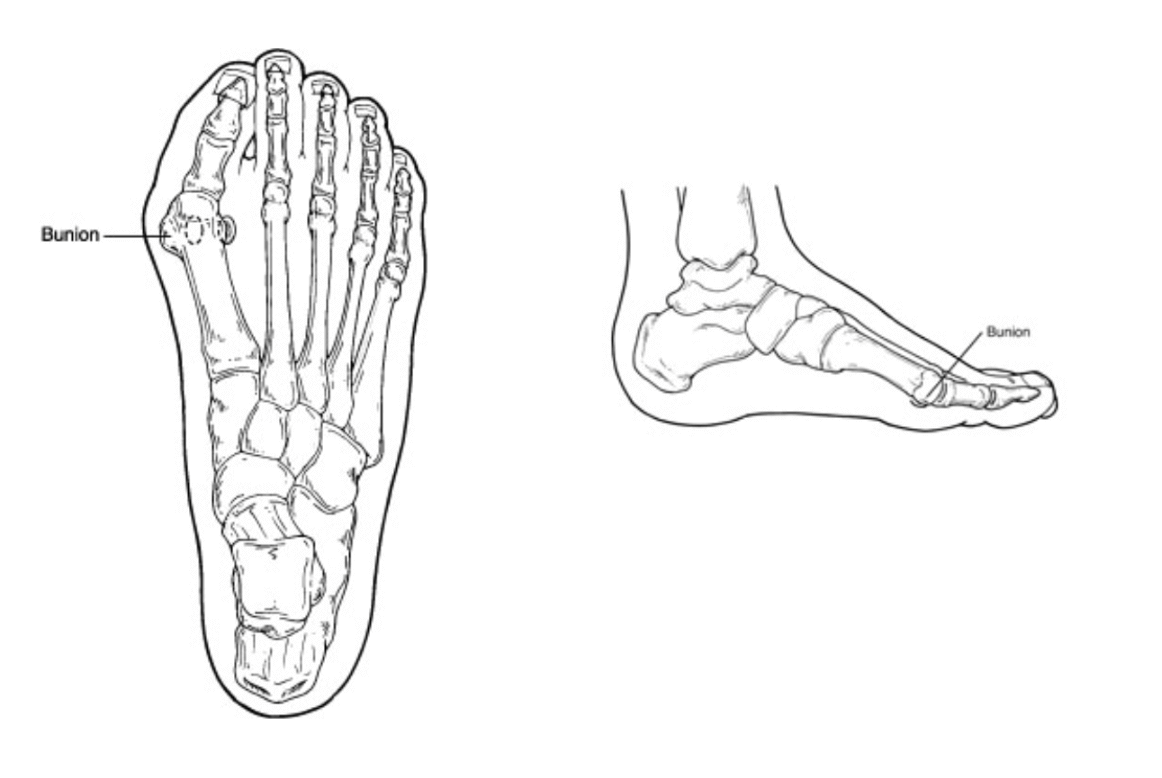
Bunions can make life difficult. They can get in the way of exercising and other activities that we enjoy. They can make shoe choices impossible and cause pain daily. This often leads to patients needing surgical intervention to remove the bunion. The Lapiplasty is revolutionizing bunion surgery and creating great outcomes for patients that need to have their bunion removed.
I encourage anybody that is deciding to have their bunion removed to see a surgeon that has experience with Lapiplasty. I have been operating on bunions for over 15 years and have seen the evolution of bunion surgery. I have seen minimally invasive surgery trends; I have seen open surgery trends and now over the last 5 years have seen Lapiplasty move to the forefront. Lapiplasty is different from other bunion surgeries in many ways.
The Lapiplasty addressed the root cause of a bunion. Bunions are created when we have an unstable foot and joint. The Lapiplasty works at the apex of the bunion deformity and at the same addresses the mechanical instability of the foot. It has proven to have great long term outcomes and will soon be the most common bunion surgery correction technique.
If you would like a consultation on your bunion I can help. Call to make an appointment with me at 425-391-8666 or contact us online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Treatment Options for Hammer Toes
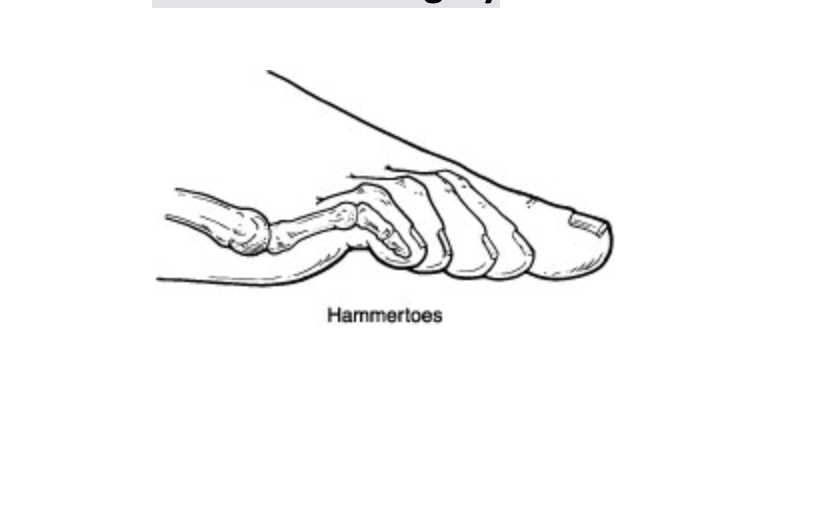
Hammer toes refer to a curling downward of the toes. This can occur in one or more toes and can be a stand-alone pathology or with another type of foot condition like a bunion. The hammer toe is often caused by shoe gear choices, trauma or inherited from mom and dad. It typically gets worse with time and makes it hard to exercise or fit in shoes properly.
The conservative options for hammer toes can sometimes relieve pain. These options are such things as wearing larger or wider shoes, taping the toes, or using pads or spacers. It is important to note that this does not fix the hammer toe. Additionally, with time it usually gets worse and the toe curls more.
Long term or surgical correction is the usuals course for most patients. This involves addressing the underlying causes of the hammertoe or toes. It is important to look at the overall foot structure and any contributing factors. The surgical procedure to correct a hammer toe can be removal of a bone or removal of a bone and soft tissue balancing. Sometimes it requires pinning of the hammer toe to allow the new position to heal and correct itself.
If you would like a consultation on your hammer toes I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses The Lapiplasty Bunion Procedure
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses The Lapiplasty Bunion Procedure
Bunion and bunion pain affects millions of people per year. It creates pain around your big toe and can decrease quality of life. The pain can become so intense or make it difficult to wear shoes often people would like it removed. Bunion surgery has been around for over 100 years however recently a new technique called the Lapiplasty has changed the recovery times and improved outcomes.
The lapiplasty is a 3-D bunion correction system that has helped to address the bunion at its origin. This procedure works to stabilize the foot and realign the metatarsal bone. It has been shown to have very low recurrence rates and great long-term outcomes.
There are a few reasons it has proved to be a game changer. One, is correcting the bunion deformity by fixing both the angular and rotational deformity of the bunion. Two, it has a faster recovery over the traditional bunion surgery. Three, it reduces complications including stiffness and improved joint stability.
I have found this new system to be revolutionary for my patients. I find it to be the future of bunion surgery. If you would like a consultation on your bunion I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Dr. Timothy Young, a Board Certified Foot Surgeon, Discusses My Top 5 Reasons Why I Recommend the Lapiplasty Bunion Repair
Dr. Timothy Young, a Board Certified Foot Surgeon, Discusses My Top 5 Reasons Why I Recommend the Lapiplasty Bunion Repair
Introduction
Bunions can be painful and disruptive, affecting the quality of life for many individuals. Traditional bunion surgery, also known as a bunionectomy, has been the standard approach for decades. However, in recent years, a groundbreaking surgical technique called Lapiplasty has emerged as a game-changer in the field of bunion repair. Surgeons worldwide are increasingly recommending Lapiplasty for several compelling reasons. In this blog, I will review the top 5 reasons why I recommend the Lapiplasty Procedure for bunion surgery.
1. Superior Three-Dimensional Correction
One of the most remarkable aspects of Lapiplasty is its ability to correct bunions in three dimensions, addressing the root cause of the deformity. Traditional bunion surgery often focuses on the visible bony bump, leaving the underlying bone misalignment uncorrected. Lapiplasty, on the other hand, repositions the metatarsal bone, restoring its proper alignment in all three planes—sagittal, transverse, and frontal. This three-dimensional correction not only provides better cosmetic results but also reduces the risk of bunion recurrence, making it a preferred choice among surgeons.
2. Faster Recovery and Reduced Downtime
Lapiplasty's minimally invasive approach and stable fixation results in faster recovery times for patients. Unlike traditional bunion surgery, which often requires patients to remain off their feet for an extended period, Lapiplasty allows patients to bear weight on their feet and start walking within days. This accelerated recovery can significantly improve a patient's overall experience and quality of life during the healing process.
3. Long-Lasting Results
Surgeons recommend Lapiplasty due to its track record of providing more durable and longer-lasting results. Traditional bunion surgery may offer temporary relief, but recurrence rates can be high. The Lapiplasty's comprehensive correction of the deformity decreases the likelihood of bunions returning, allowing patients to enjoy a more permanent solution to their foot pain.
4. Stable Fixation
The Lapiplasty utilizes very stable plates. These allow earlier weightbearing and return to activities. This fixation helps to promote optimal bone healing and long term stability. Surgeons who recommend Lapiplasty often highlight the fixation benefits of this innovative technique, which can boost patients' confidence and satisfaction with their results.
5. Evidence-Based Success
Surgeons have confidence in recommending Lapiplasty due to the strong evidence supporting its success. Numerous clinical studies and real-world cases have demonstrated the effectiveness of this procedure in addressing bunions, relieving pain, and improving patient outcomes. These data-driven results reassure both surgeons and patients that Lapiplasty is a reliable and proven treatment option.
Conclusion
Lapiplasty has revolutionized the field of bunion repair with its three-dimensional correction, quicker recovery times, long-lasting results, stable fixation, and evidence-based success. Surgeons worldwide recommend Lapiplasty as a superior alternative to traditional bunion surgery for patients seeking a more comprehensive and permanent solution to their foot pain. If you're considering bunion repair, please contact my office so I can evaluate your specific needs and discuss the benefits of Lapiplasty as a potential solution to your bunion woes.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr Brandon Nelson, A Board Certified Physician and Surgeon, Discussed When Your Heel Pain Will Not Go Away and You Need A Second Opinion

Heel pain can be difficult for patients and physicians alike. It can provide a challenge for all parties involved. I have seen hundreds or maybe even thousands of second opinions for heel pain. Over the years I have learned many valuable lessons that can be extremely beneficial to treating heel pain.
One of the first lessons I learned was to listen to the patient. Often patients provide great clues to the cause and origin of heel pain. The history and story a patient tells often paints the perfect picture for how the pain is continuing to cause discomfort. Not all heel pain is the same and although plantar fasciitis is the number one cause remain open to other sources. This leads me to lesson number two.
Lesson number two not all heel pain is plantar fasciitis. I have seen so many other causes and as a provider we need to be diligent. The back can be a source of chronic heel pain. Patients with back issues can have manifestations in the feet. Another common cause is nerve pain. Over the years I would say this is the most common reason heel pain does not get better. The clinician is missing a nerve entrapment. This is not all of the other reasons for heel pain but a few examples to illustrate the importance of recognizing there are other sources of heel pain.
Lesson three is to understand not all heel pain can be treated the same. I have seen patients over the years that have similar heel pain but similar treatments do no work. This is why it is important to treat all patients as individuals. To make sure to look at foot structure, gait cycles and daily routines to see how each individual can be treated for the best possible outcome.
If you have heel pain and are in need of a second opinion or are just fed up with daily pain make an appointment with me today I can help. Give us a call at 425-391-8666 or make an appointment online.
Sincerely,
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses Why the Lapiplasty Procedure for Bunion Surgery Is His Preferred Method
Bunion surgery has been around for over 100 years. There are many techniques that have been utilized for correction of a bunion. The majority involve cutting a bone and realigning a joint. The goal of these surgeries are to straighten the 1st metatarsal and eliminate the deviation of the bone. Today with new research and modern technology we have a better understanding of function anatomy and have begun to look at bunion surgery outcomes. This has led the majority of us surgeons to utilizing the Lapiplasty technique for better long term outcomes.
I personally have been a Lapidus surgeon for over 15 years. I trained in the Northwest and have had the opportunity to work with some of the pioneers of bunion surgery. We have seen through research that the Lapidus procedure holds up the best over time. The long term outcomes show very little recurrence and better overall patient happiness. The lapiplasty system has allowed us to take the lapidus bunion procedure and make it more reproducible.
Lapiplasty is a system created by Treace Medical that has taken some of the technically challenging parts of the lapidus bunionectomy and simplified them. It has a system of cutting jigs and guides that make it simple to correct the bunion. I find patients are extremely happy and have seen incredible long term results. If you have a bunion schedule and appointment with me, I can help you review your options. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses How To Best Treat Your Morton’s Neuroma

Morton’s neuromas can be extremely painful for many people. I think nerve pain is one of the most challenging pathologies to treat. I see quite a few patients each week with neuromas. I find there are a few things that can make a big difference in neuroma pain. Let’s review them and see if we can help you if you are experiencing nerve pain or neuroma pain.
Neuromas are very susceptible to alcohol injection therapy. This is one of the best available treatment options we have currently. This technique has been around for about 30 years and the literature reports an average success rate of 89%. I have been utilizing it now for about 15 years and find it highly effective for patients. The average patient needs 4-6 injections about 2 weeks apart. I have even had great success with stump neuromas and patients that have tried many other conservative treatments.
Orthotics can be a big help as well. I am not talking about a shoe insert, or something over the counter or at a shoe store. These are prescription orthotics devices made by a physician. A gait analysis and overall biomechanical examination needs to be done to identify causes contributing to the nerve irritation. I like to utilize a 3-D scan of the foot to get an extremely accurate copy of the foot structure. I find active people do well with these devices and find significant pain relief.
Nerve supplements and laser, FDA approved laser, can also be used to help nerve pain. We currently have a laser that has shown extremely promising results with no complications. I like to combine nerve supplements with laser and infra-red-light therapy. The best part of this is no interference with any other medications, no down time, and no side effects.
If you have a neuroma, I can help, call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Timothy Young Discusses What to Expect After Lapiplasty Bunion Surgery: Road to Recovery
.jpg)
Dr Timothy Young Discusses What to Expect After Lapiplasty Bunion Surgery: Road to Recovery
Introduction
Bunions, those painful bony bumps that form at the base of the big toe, can be incredibly uncomfortable and limit your mobility. For those who have chosen to undergo bunion surgery to alleviate the pain and discomfort, it's important to be well-prepared for what comes next. In this blog, we'll discuss what to expect after bunion surgery including Lapiplasty bunion surgery and provide insights into the recovery process to help you make the journey as smooth as possible.
Day of Surgery
1. Arrival at the Surgery Center: On the day of your surgery, you'll arrive at the surgery center, where you will be prepped for the procedure. The medical team will ensure you're comfortable and informed about the process.
Anesthesia: Bunion surgery is typically performed under local anesthesia with sedation. You'll discuss this with your surgeon before the procedure.
The Surgical Procedure: The surgery usually takes approximately 2 hours, depending on the complexity. The surgeon will make incisions, remove the bunion, and realign the toe joint. With the Lapiplasty procedure there will be 2 plates. With some the other Lapidus procedures there may be 2 or possibly 3 screws.
Recovery Timeline
1. Post-Operative Recovery Room: After the surgery, you'll spend some time in the recovery, where the medical staff will monitor your vital signs and ensure you're comfortable.
Returning Home: Most patients return home on the same day of surgery.
The First Weeks After Surgery
1. Pain Management: Expect some pain and discomfort, which is normal after bunion surgery. Your surgeon will prescribe pain medication to help manage this. Follow their instructions carefully.
Swelling and Bruising: Swelling and bruising are common. You can use ice packs and elevate your foot to reduce swelling.
Dressings and Bandages: You will have a dressing on your foot to protect the incision. Keep it clean and dry. Your surgeon will give you instructions on when to change the dressings.
2. Weight-bearing timeline. This varies from patient to patient.
First 2 weeks with the Lapiplasty typically you are using a scooter or crutches and keeping weight off.
Week number 3 – 6 you progressively bear weight with your boot.
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Burning Pain in Your Heel

Have you experienced burning in your heel? Does your heel feel like it is on fire? Are you getting pins and needles in your heels? This could be a condition called Baxter’s neuritis or an entrapped nerve in your foot. This can often be confused with plantar fasciitis and the two can be difficult to distinguish.
I saw a few patients this last week that had Baxter’s neuritis and it made me want to write a few words about it. This condition was brought to popularity by Dr Baxter and prior to that this pathology was often thought of as plantar fasciitis. It should be noted that many patients I see have both conditions present. The most notable difference seems to be the burning pain and radiating nerve pain that can be reproduced by tapping the nerve. However, a nerve study can be helpful to confirm the diagnosis and help with planning treatment.
There are a few conservative measures that can provide pain relief. Orthotics, injections, and some medications prove to be successful. However, some patients do not find any improvement and surgical decompression of the nerve is done at that point. The constricting structures around the nerve are freed up and the pain typically resolves. I always recommend trying conservative measures first before considering surgical intervention.
If you have burning heel pain I can help, call to make an appointment with me at 425-391-8666 or schedule an appointment online.
carpet cleaning seattle
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, Discusses the Lapiplasty Procedure for The Best Possible Correction of a Bunion
Dr Brandon Nelson, Discusses the Lapiplasty Procedure for The Best Possible Correction of a Bunion
Bunions can be quite painful for people especially as they get larger and make it difficult to fit in shoes. Bunions tend to get bigger as time goes on and eventually push the other toes out of alignment. But what can be done to stop the bunion or even slow it down?
Many people want to know what can be done from a conservative standpoint to slow a bunion. I have seen all sorts of devices to pull the toes around to try and straighten a bunion. But, it should be known that the bunion is a bony pathology that is related to a change in position of the bone. This makes it impossible to apply something to the outside of the foot to fix a bone on the inside. However, there are a few things that can slow down a bunion. Most important is to understand a bunion gets larger the more pressure that is exerted on it.
Meaning the more you walk the bigger the bunion gets. This is where conservative therapy begins. The best now measure to intervene here is a prescription orthotic for bunion correction. I am not talking about an insert from a shoe store or online this must be done by a physician. This is a prescription medical device where biomechanical measurements and 3-D measurements of the foot are taken. The good news about this is most insurances cover this device as long as it is prescribed by your foot and ankle physician.
Surgical correction is the ultimate stop gate to the bunion getting bigger. There are many options for surgical correction but the one moving to the forefront of medicine today is the Lapiplasty. This procedure is based upon the Lapidus which has been utilized for almost 100 years. This is a tried and true method for getting amazing bunion correction and providing lasting results. If you have a bunion I can help. Give me a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson



