bfdadmin
bfdadmin
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Neuroma Treatments
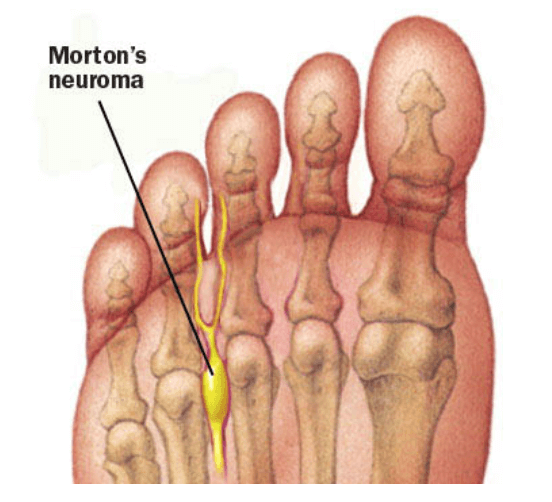
Dr. Timothy Young, a board-certified foot surgeon, discusses neuroma treatments:
Our Doctors have been using Alcohol injections for Morton's Neuroma for over 10 years with excellent success. Most patients have between 6 - 8 injections at weekly intervals. Occasionally a "mini-series" will be done after 12 months. For most patients, there is minimal discomfort after the injections and there is progressive relief from the Neuroma symptoms.
We typically use between 20-30% dehydrated alcohol. Ultrasound guidance is critical for correct injection technique. Most frequently we treat the 3rd intermetatarsal space, and runner up is the 2nd intermetatarsal space. This provides an excellent alternative to surgical treatment, and we also treat stump neuroma problems (where there is reoccurrence of the neuroma symptoms after prior foot surgery).
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr. Brandon Nelson, A Board Certified Physician and Surgeon, Discusses the American College of Foot and Ankle Surgeons Consensus on Bunions

Dr Brandon Nelson, A Board Certified Physician and Surgeon, Discusses the American College of Foot and Ankle Surgeons Consensus on Bunions
This month the American College of Foot and Ankle Surgeons released an updated version of statements regarding bunion deformities. It was released to look at the best available evidence, clinical practice, and clinical experience to treat bunions. As a member and Board-Certified Surgeon, I feel it is an essential tool to have in our clinical practice. I will summarize some of the important findings:
1. The bunion is a deformity that should be considered chronic, progressive, and degenerative in nature.
2. The juvenile bunion should be evaluated and managed differently than the adult.
3. Effective assessment and evaluation require and x-ray.
4. Procedural decision making for bunions should address the specific anatomy of the deformity.
5. Bunions should always be addressed with joint preserving procedures when appropriate.
This is a main summary of what was stated. Bunions continue to be a difficult pathology for patients. If you have bunion pain I am happy to help come up with a treatment plan. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr. Timothy Young, a Board Certified Foot Surgeon, Discusses Collagen Supplements After Surgery
Dr. Timothy Young, a Board Certified foot surgeon, discusses collagen supplements after surgery.
For example Achilles tendon surgery or repair of an Achilles tendon rupture. Peroneal or posterior tibial tendon surgery. In addition zinc (25 mg up to 50 mg per day) and boron (3 mg per day) are supplements the can be helpful with deep tissue healing and wound healing. It's important to note that zinc can compete with some other essential elements such as calcium and magnesium so it's best to take zinc by itself for example at lunchtime. Remember there are always things that you can do to help your body heal.
If you are experiencing foot or ankle pain, please give us a call at 425-391-8666 or make an appointment online today.
Dr. Brandon Nelson, A Board-Certified Surgeon & Physician, Discusses Morning Foot Pain
Getting out of bed in the morning and having foot pain has to be one of the worst ways to start your day. There was a period of time where I have suffered from this condition and found it extremely frustrating in the morning and disheartening to start that way.
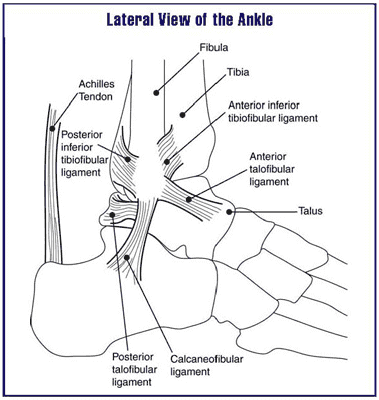
There are many different causes of morning foot pain and the most common cause can be a tight Achilles tendon. I cannot stress the importance of stretching your Achilles tendon throughout the day whether or not it’s on stairs or against a wall. The Achilles tendon is the most overused tendon in the human body and very rarely has time to rest. Therefore it is extremely important to maintain flexibility of the Achilles tendon and work on improving ankle range of motion.
To help resolve morning heel pain one can use a belt or theraband to work on ankle range of motion. I encourage you to use these devices to fully stretch your toes towards your nose and really stretch out the back of the ankle. Another great exercise is to use your ankle to write the alphabet a few times before getting out of bed. Additionally getting into slippers or recovery sandals can be successful in alleviating some of the morning pain.
These are just some gentle general recommendations and I encourage anybody with chronic pain evaluated by a physician before therapy. There are cases where any stretching or activities can cause increased pain or dysfunction.
Sincerely,
Dr. Brandon Nelson, A Board Certified Foot & Ankle Surgeon and Physician, Discuss Big Toe Pain

The big toe or 1st metatarsal phalangeal joint is one of the major weight bearing joints in the foot. It is utilized in the normal gait cycle and normal supports approximately 80% of the body weight with each step. With the average person walking 110,000 miles in a lifetime this can be quite a challenge if you are experiencing toe pain. There are a few major causes of toe pain and we will discuss a couple today, arthritis and bunions.
Arthritis of the big toe is caused from normal wear and tear of the joint or from a sustained injury. This can result in losing cartilage in the joint and a person begins to experience pain and swelling. The toe joint can often enlarge and every step can become painful. An x-ray is extremely helpful in establishing a diagnosis and a treatment plan. This is a common pathology of the 1st MTPJ that causes arthritis called Hallux Limitus. This is a result of abnormal pressures in the joint and can progress with time. There are quite a few options available to help this condition.
Bunions are another common reason a big toe can be painful. With a bunion you will see the toe is deviated and often appears to have a large bump. Most people will have a family history of bunions. Bunions as well become larger with time and increasingly painful. Again, an x-ray can be helpful for coming up with a treatment plan. A large majority of bunions end up requiring surgery to fix.
If you are having big toe pain, I can help. Give us a call at 425-391-866 or make an appointment online today.
Sincerely,
Dr. Brandon Nelson, A Board-Certified Foot & Anke Surgeon and Physician, Discusses Bunion Surgery
.jpg)
We know that bunions are an inherited trait that can be exacerbated by activities and shoe gear. Patients can have a bunion on the inside or outside of their foot. The typical bunion is on the inside of the foot and involves the 1st metatarsal while the bunion on the outside of the foot involves the 5th metatarsal. Either pathology can often require surgical intervention in order to provide long term relief and the primary surgery is usually the bunion on the 1st metatarsal. The bunion will usually dictate the recovery and the bunion on the 5th metatarsal usually heals faster.
Bunions are typically fixed in a few ways, either a surgery at the head of the metatarsal or the base of the metatarsal. It is important to get an x-ray to examine the overall foot structure to make sure there are no other driving forces that need to be fixed. The typical foot structure we see with a bunion on both sides is a flat foot that has progressed with time. The foot often widens when a flatfoot is present to try and create more stability. The flatfoot may or may not need to be addressed.
Most bunion surgery patients will be walking the entire time after surgery and can continue with modified exercise. I utilize techniques that allow my patients to be more active and recover faster. It takes years and hundreds of patients to perfect these techniques and dealing with athletes has allowed an advantage to improve on outcomes. If you are having bunion pain please make an appointment and I will see how we can best help you. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Board Certified Surgeon & Physician
Dr Brandon Nelson, A Board-Certified Physician and Surgeon, Discuss How To Best Treat Your Heel Pain

Heel pain is the most common presenting pathology at my practice. In general, I would say 1 out of every 6 patients is for heel pain. This can be common for both adults and children. The adult usually has heel pain that is caused by plantar fasciitis and for children this is usually apophysitis or Sever’s disease.
Adult heel pain is common as one starts an exercise program or as our mileage on our feet increases. The symptoms usually begin with pain in the morning or after a walk. The feeling is often described as a bruised sensation or a burning pain. It is important to identify the underlying causes and address these. I do think an x-ray is warranted and the earlier the treatment the better.
Children usually seem to have heel pain between the ages of 10-14. The typical child has been playing sports, especially cleated sports. They usually describe a soreness that can result in limping. It is again important to take an x-ray and for underlying foot conditions.
Both plantar fasciitis and apophysitis seem to be most common in certain foot structures. These include flatfeet and tight Achilles’ tendons. I recommend stretching the calf for the tight achilles. However, the flatfoot needs to be thoroughly evaluated to prevent long term issues. I really enjoy treating both of these conditions and have great long-term protocols to eliminate this pain once and for all.
If you or your child is suffering from heel pain please call so I can help. Make an appointment online or give us a call at 425-391-8666.
Sincerely,
Board-Certified Foot & Ankle Physician & Surgeon
Dr Brandon Nelson, A Board-Certified Physician & Surgeon, Discusses The Newest Bunion Surgery Technique

Bunions can be quite painful for many people. They can begin to interfere with activities and make exercising difficult. Additionally, it can become difficult to find shoe gear that fits properly. Most bunions are a genetic condition that is inherited and develops with time and loading of the foot. Many bunions get bigger as time goes on and eventually require surgical repair. Surgery for a bunion can be broken down into two categories what are called head procedures and base procedures. Today I will only discuss a base procedure as this seems to be the most common question lately.
Base procedures are often used for large bunions and can be a powerful tool to correct the foot. The base procedure is usually further divided into joint sparing procedures and joint destructive procedures. The most asked about procedure currently is the Lapiplasty. The Lapiplasty is a procedure based off a technique described by Paul Lapidus. It involves removing a joint in the foot that is the apex of the bunion deformity. The reason this procedure is so effective is it eliminates the primary cause of the bunion, the hypermobile joint that initiated the development of the bunion.
Lapiplasty is a tool set that is provided to make the Lapidus bunion surgery easier. This is a technique that has been utilized for years however this instrument set is the first of its kind and has helped make this procedure more reproducible. This is the most common bunion procedure I execute as it has great correction and great long-term outcomes. If you have a bunion and would like a consultation, make an appointment today and I can help.
Give us a call at 425-391-8666 or make an appointment online.
Sincerely,
Board Certified Physician and Surgeon
Dr. Timothy Young, Board Certified Foot and Ankle Surgeon, Talks About Hallux Limitus Surgery
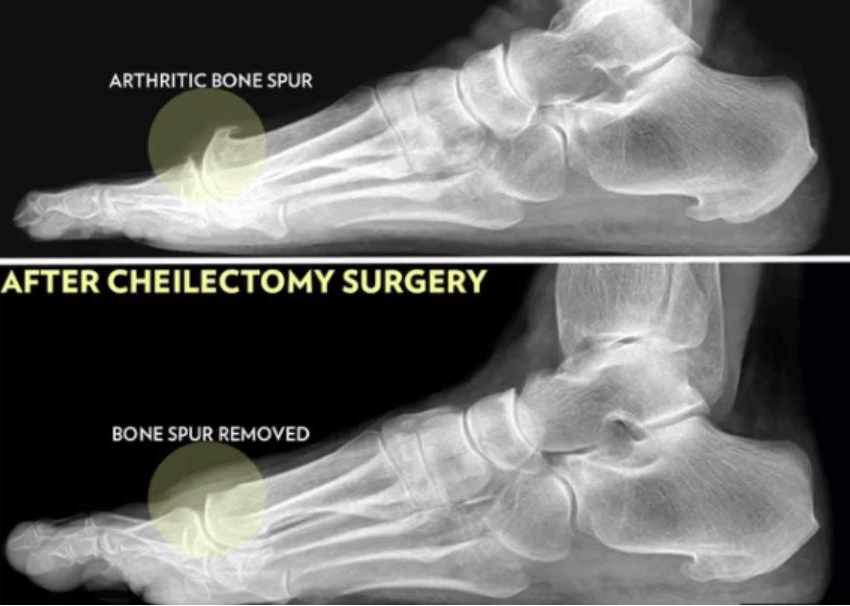
Dr. Timothy Young, board certified foot and ankle surgeon, talks about hallux limitus surgery for arthritic bone spur removal of the great toe.
Arthritis of the great toe is very common. Usually there is excessive compression on the top of the joint, and over months to years, painful bone spurs or osteophytes can develop. These create even more pressure and pain, and there is often bone on bone contact between these bone spurs. Removal of the bone spur is a very effective treatment for this problem. This surgery is called a cheilectomy. Cheilectomy surgery for arthritis of the great toe is quite straightforward and has a rapid recovery. Cheilectomy surgery is the most basic and simple procedure, from a surgical perspective for this condition.
There are more and fall procedures that can be done such as a decompression osteotomy of the bone, or fusion of the joint. These procedures usually require significant additional protection and recovery time. The surgical procedure itself involves access to the joint with an incision through the tissue layers including the joint capsule. The bone spurs are then exposed and removed surgically. This also involves using a surgical bur to smooth down the top of the joint. It is quite common to fine small loose fragments of bone, which are also removed during the procedure. If there are loose flaps of cartilage, and failure removed and the exposed bone can be drilled to create a fibrocartilage patch.
The joint and wound is flushed and then the layers are repaired and sutured. Recovery involves using a surgical shoe or cast boot. Initially putting weight on the heel for the first few days, and after that for weight with a surgical shoe or cast boot works well. Sutures are typically removed 2 weeks after the surgery. Most of our patients stay in the boot for 3 weeks.
If you are experiencing foot and ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr Brandon Nelson, A Board Certified Foot & Ankle Physician and Surgeon, Discusses Hammer Toes
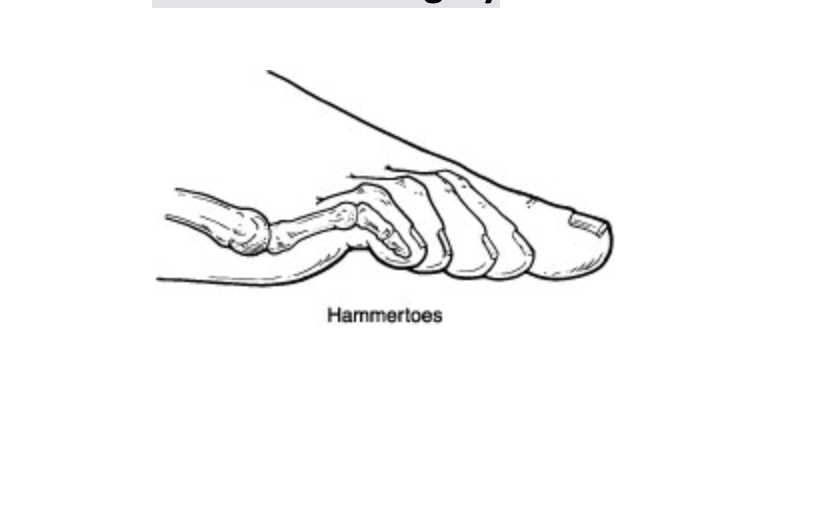
Hammer toes are a condition that affects usually multiple toes in the foot. This condition can occur on one foot or both. It is often part of an overall deformity of the foot for example a bunion with hammer toes is common. There tends to be a family history of hammer toes and pain can begin as the condition worsens. Often patients will present with pain from shoe gear rubbing or pain with activities like running. The hammer toes are a progressive deformity and I encourage early intervention to manage the deformity.
The most common cause of hammer toes is the foot trying to stabilize itself. Often the long flexor tendons of the foot are working to create an arch or support the arch. Patients often have a flatfoot associated with this pathology and the hammer toes start to progress as the foot becomes flatter. The foot works hard to try and stop the flattening and the flexor tendons begin to overpower the digits. The digits begin to curt and hammering is the result.
The only long-term fix of hammer toes is surgical. The procedure itself is relatively straightforward and quick. It involves removing a piece of bone and often lengthening a tendon or releasing some soft tissues. It is a stepwise approach to the hammer toe that provides the best long-term outcomes. I have patients that choose to have it done with just some local anesthetic and the recovery is uneventful.
If you are suffering from curling digits and need an evaluation I can help. Please contact the office at 425-391-8666 or make an appointment online today.
Sincerely,
Board Certified Physician and Surgeon



