foot surgeon issaquah
Displaying items by tag: foot surgeon issaquah
Dr. Timothy Young, a Board-Certified Foot Surgeon Discusses: Potential Risks Associated With Bunion Surgery.
 Understanding the Potential Risks of Bunion Surgery
Understanding the Potential Risks of Bunion Surgery
Bunion surgery, also known as bunionectomy or hallux valgus correction, is a common procedure used to correct deformities of the big toe joint. While this surgery can provide significant relief for individuals suffering from bunion-related pain and discomfort, like any surgical procedure, it carries certain risks. Understanding these potential risks is essential for individuals considering bunion surgery.
1. Infection
One of the primary risks associated with any surgery is the possibility of infection. Although steps are taken to minimize the risk, such as sterile operating environments and antibiotics, infections can still occur. Symptoms of infection may include redness, swelling, warmth, and discharge at the surgical site. Prompt medical attention is necessary if infection is suspected. Note that we recommend patients scrub the foot with chlorhexidine the night before surgery and the morning of surgery. Prophylactic antibiotics are often given during the surgery via intravenous route to help reduce the risk. Leaving the initial dressing intact and making certain that it does not get wet are also very important.
2. Nerve Damage
During bunion surgery, there is a risk of nerve damage, particularly to the nerves surrounding the big toe joint. This can result in numbness, tingling, or altered sensation in the toes or foot. In most cases, nerve damage is temporary and resolves over time, but in rare instances, it may be permanent. With the Lapidus or Lapiplasty surgery the dorsal medial cutaneous nerve of the foot is often encountered. It is not always possible to retract the nerve and therefore this nerve may have reduced function or sensitivity after surgery.
Some individuals may experience delayed healing after bunion surgery. Factors such as age, overall health, and the extent of the surgical procedure can affect healing time. Delayed healing may result in prolonged pain, swelling, and limited mobility in the foot. Delayed healing can relate to the incision itself, the subcutaneous layers and capsule – soft tissue, and finally bone. Anyone of these layers can be affected by delayed healing. In general the most critical is bone healing because once the bone healing is adequate and stable then protected and/or limited weight-bearing is not necessary.
4. Recurrence
While bunion surgery aims to correct the misalignment of the big toe joint, there is a risk of recurrence. Factors such as genetics, foot structure, improper footwear, and post-operative care can contribute to the recurrence of bunions over time. Additional surgical interventions may be necessary if a bunion returns after initial correction. The more severe the bunion, and the younger the patient is at the onset of the bunion (juvenile bunion) may also make the patient more prone to reoccurrence. Therefore it is critical to make sure that your surgeon that is the most correct the procedure possible in these cases.
5. Stiffness and Reduced Range of Motion
After bunion surgery, some individuals may experience stiffness and reduced range of motion in the affected toe or foot. Physical therapy and exercises may be recommended to improve flexibility and mobility. In severe cases, stiffness may persist despite rehabilitation efforts. The more work that is done directly involving the great toe joint and the first metatarsal phalangeal joint (first MTP joint) and its capsule, the more tendency there will be to have stiffness of the great toe joint here. In some cases such as with the Lapidus or Lapiplasty procedure it is possible to have excellent correction with minimal surgical involvement or dissection of the first MTP joint capsule. These patients seem to have better flexibility postoperatively.
6. Blood Clots
There is a risk of developing blood clots (deep vein thrombosis/DVT) after any surgical procedure, including bunion surgery. Blood clots can be dangerous if they travel to the lungs (pulmonary embolism). To reduce the risk of blood clots, patients may be advised to move their legs regularly after surgery and wear compression stockings. In addition there are a number of other factors that can make patients prone to a DVT. Some examples are estrogen medications and/or supplements, genetic history of bleeding disorders, smoking, the use of the tourniquet during surgery are all examples of risk factors.
7. Allergic Reactions
Rarely, individuals may experience allergic reactions to medications, anesthesia, or materials used during bunion surgery. It is essential to inform your healthcare provider of any known allergies before the procedure to minimize this risk.
8. Unsatisfactory Results
Despite the best efforts of the surgeon, some individuals may be dissatisfied with the results of bunion surgery. This can occur if the desired correction is not achieved, or if complications arise during the healing process. Revision surgery may be considered in such cases.
Reducing Risks and Ensuring Successful Outcomes
While the risks associated with bunion surgery cannot be entirely eliminated, there are steps individuals can take to reduce these risks and improve the likelihood of a successful outcome:
Choose a Qualified Surgeon: Select a board-certified surgeon with experience in bunion surgery.
Follow Preoperative Instructions: Adhere to preoperative instructions provided by your surgeon, such as avoiding certain medications and fasting before surgery.
Understand the Procedure: Take the time to understand the bunion surgery procedure, including potential risks and expected outcomes.
Follow Postoperative Care Guidelines: Follow your surgeon's postoperative care instructions, including medication management, wound care, and rehabilitation exercises. Make sure you get clear postoperative instructions and really plan out your postop help and routine. For example how will you get around and who will help with food. First 48 hours postoperatively, it is critical to have somebody immediately available.
Attend Follow-Up Appointments: Attend scheduled follow-up appointments with your surgeon to monitor healing progress and address any concerns promptly.
By being informed about the potential risks of bunion surgery and taking proactive measures, individuals can help minimize complications and achieve a successful outcome from their surgical procedure. Consulting with a qualified healthcare professional is crucial for personalized advice and guidance regarding bunion surgery and its associated risks.
If you have any questions or would like a consultation please call 425-391-8666 and make an appointment online.
Dr. Timothy Young
Foot & Ankle Surgeon
Issaquah's Top Podiatrist
Dr. Timothy Young, a Board-Certified Foot Surgeon Discusses Tendinosis
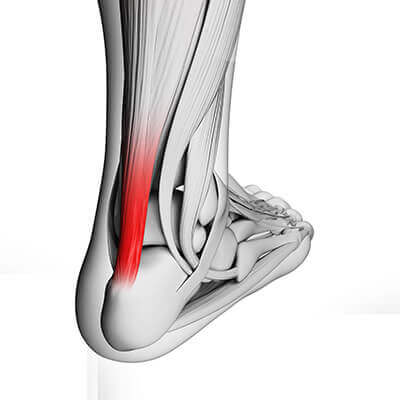
The most effective treatments for this include prescription orthotics to address the mechanics and to reduce the mechanical shearing within the tendon. Calf stretching and a night splint can be very effective. KT tape is a useful adjunct for this problem. Shockwave therapy is extremely helpful for this condition. Some individuals will require surgery for this. This can involve removing some of the damaged portion of the tendon, and it can also involve lengthening the tight calf muscle with the gastrocnemius recession.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Removal of Hardware After Foot Surgery

Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Removal of Hardware After Foot Surgery.
Sometimes there is bone overgrowth, and this requires a larger incision and bone removal. This would happen typically if it h been more than one or two years after the original surgery. Prior to surgery using x-ray or ultrasound imaging one can plan ahead of time and allow for a much smaller surgical incision and therefore a much quicker postprocedure recovery. In these cases often just one simple suture or Steri-Strips is all that is necessary for wound repair. In the case of screws where there has been bone overgrowth, or plates the larger incision has to be made.
Therefore, there will be more wound healing and additional sutures required. In the case of hardware removal with just several small screws and small incisions, often there can be returned to activity within a week. If it is a larger procedure as described above involving a plate or bone overgrowth, then there may be a longer recovery of two weeks or even longer. Another intraoperative tool that we have within our ASC is fluoroscopy. Fluoroscopy can help locate hardware if there has been bone overgrowth or other factors making it difficult to find hardware during surgery.
If you are experiencing any foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, a Board-Certified Foot Surgeon Discusses Digital Foot Surgery.
Dr. Timothy Young, a Board-Certified Foot Surgeon Discusses Digital Foot Surgery.
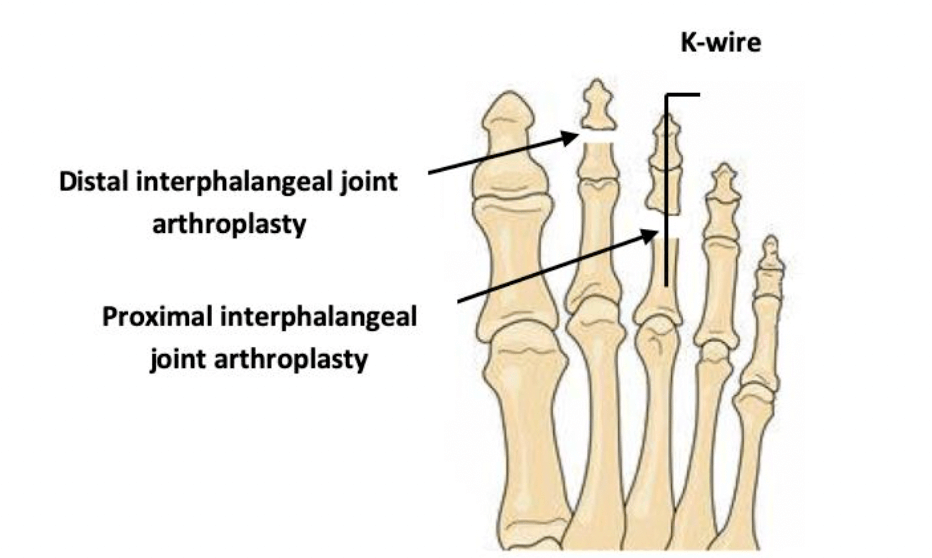
Sometimes during toe surgery, a pin will stick out the end of the toe. And other times, the pin will be buried or covered with skin. As we've discussed previously, it is common to use a K wire or pin during hammertoe surgery or other digital foot surgery. Often times the pin will stick out of the tip of the toe and be visible. When this is done it is very easy when the time is appropriate, for your surgeon to remove the K wire without making an incision in your toe. The advantage to having the K wire covered with skin or buried is that there is no direct pathway for bacteria to travel from the pin into the toe.
Therefore it is okay once you incision has healed to get your foot wet with the buried K wire, but that is not possible when it sticks out of the toe. Also the K wire can be left in this buried position for a longer period of time without pin track irritation or infection. The disadvantage of a buried K wire is that removal will require a minor procedure to remove the pin. Sometimes because there is such a thin fat pad at the tip of the toe, it's difficult to get enough tissue or skin to properly.
If you are experiencing foot or ankle pain, please give us a call at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Why Toes Are Often Pinned During Foot Surgery
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Why Toes Are Often Pinned During Foot Surgery
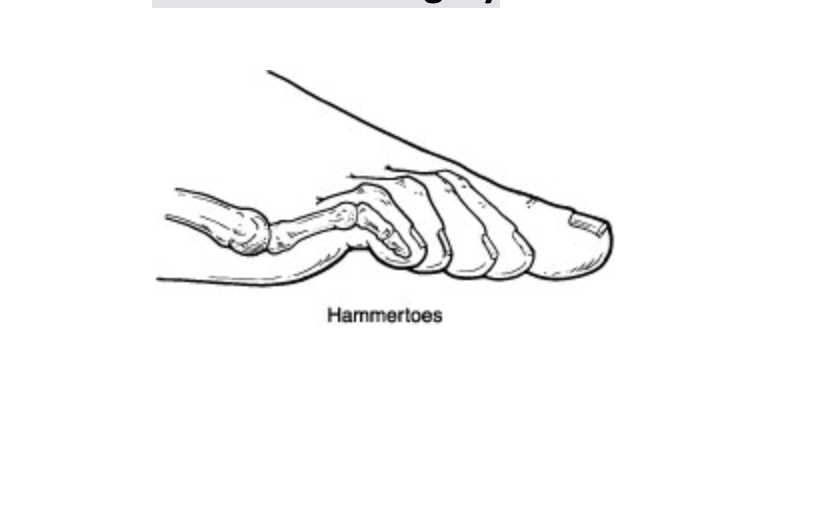
Pinning toes (with a K wire) is a common practice with foot surgery. In reality what is called a pin is a Kirschner wire or K wire. The K wire is typically is placed directly within the bones of the toe. The purpose is to hold the toe incorrect alignment. For example in other parts of the body including midfoot, ankle and leg when there's a fracture often a cast will work. But one can not effectively cast a toe. Therefore pinning a toe is an excellent option that holds it stable to allow for the correct healing and the correct alignment to be maintained during the postop time frame. For example, a patient with a hammertoe will have a contracture and adaptation of the proximal interphalangeal joint or the first knuckle within the toe.
This bone has to be surgically remodeled to allow for realignment. Once the bone remodeling is done, rather than just putting a bandage on the toe, a K wire is used in the toe to make certain that the correction and alignment are maintained exactly as necessary and so that the postoperative healing will continue in the correct alignment until that initial healing is adequate. In some cases the toe is actually fused and typically the K wire with stay in between four – six weeks. The closer to the six week timeframe, the higher correlation with long-term successful fusion.
If you are experiencing foot or ankle pain, please give us a call at 425-391-8666 or make an appointment online today.
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discusses How the Lapiplasty Procedure Works

The Lapiplasty has seen a lot of attention in recent literature. It seems to be moving to the forefront of foot surgery and is showing promising results. It has shown to be a reproducible bunion surgery that has great long term results. I find the procedure to be highly successful and utilize it weekly in my bunion surgeries.
Lapiplasty is a surgical technique and instrument set that allows surgeons to decrease operating time and help patients return to activities much more quickly. It utilizes a technique that has been proven to be one of the best corrective measures for bunions. It also provides for great fixation of a bunion and maintains flexibility of the big toe joint.
My experience with the Lapiplasty has been positive. It makes the correction of the bunion much easier and reproducible. It allows for precise bone cuts and easy options for fixation of the bone. I find it extremely helpful for young patients and decreasing the chance of recurrences. The overall recurrence rate seems to approach about 3%. If you have a bunion and would like a consultation for a Lapiplasty please contact my office. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr Brandon Nelson, A Board-Certified Physician & Surgeon, Discusses Lis Franc Injuries and Chet Holmgren
Lis Franc injuries refer to a midfoot injury that can occur when force is applied to the foot. The original injury was named for a Napoleonic Surgeon that saw quite a few soldiers fall from horse back and injure their foot. This injury now is most common in sports and can be quite devastating to the player.
Lisfranc injury is a dislocation or fracture in the midfoot area. It is very rare, however, vital that it is not missed because long-term damage can occur.
Chet Holmgren, the number 2 pick overall in the NBA draft recently injured his foot. He was drafted by the Thunder and a standout from Gonzaga, this 7 footer is expected to be a force in the NBA. He was guarding Lebron James when the injury occurred.
Click or tap to follow the link. https://www.youtube.com/watch?v=wMRyU1dkoIY.
It is clear this was a Lis Franc’s injury, and he has undergone surgery already. This will be a long recovery and he may miss the entire season. We wish this young man the best and a speedy recovery.
In my practice I see quite a few athletes that present with a delayed presentation of this injury. Typically, they will present to the ER with an injury that is diagnosed or assumed to be a sprain. However, weeks later they are still in pain and find their way to my office. Careful exam and x-ray can usually reveal this problem but sometimes an MRI is warranted. Treatment then proceeds and most patients make a great recovery depending on the severity of the injury. If you have a foot sprain and are in pain, please don’t delay and contact the office immediately at 425-391-8666 or make an appointment online.
Sincerely,
Dr. Timothy Young, a Board Certified Foot Surgeon, Discusses How to Enhance Results of Hallux Limitus Surgery with a Cheilectomy
Dr. Timothy Young a board certified foot surgeon discusses how to enhance results of hallux limitus surgery with a cheilectomy.
If you have arthritis of your great toe joint or questions about potential surgery or procedures for this please request a consultation at our clinic. Give us a call today at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, A Board Certified Foot Surgeon, Discusses Postsurgical Scar Formation and Supplements

Dr. Timothy Young, A Board Certified Foot Surgeon, discusses postsurgical scar formation and supplements.
In addition after bone is resected bone often has excellent blood flow and there can be a blood clot or hematoma on the surface of the bone, deep within the wound. This can be resorbed by the body and also can eventually convert to scar tissue and again cause ongoing swelling or stiffness to the surgical site. Two supplements may be helpful for this. One is nattokinase and the other is serrapeptase. Both of these supplements should be taken 30 minutes before food for best absorption. The nattokinase can be taken once a day and this serrapeptase can be taken twice a day. Talk to your surgeon or naturopath to further discuss the role of these supplements with your particular situation.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
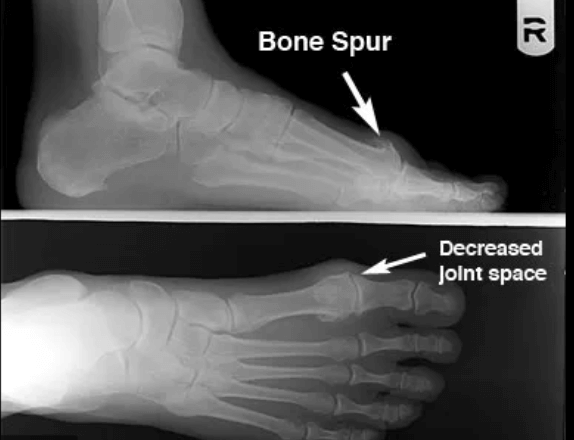
Dr. Timothy Young Talks About Minimally Invasive Foot Surgery
So it is a compromise. There are times when minimal incision surgery is extremely effective. For example smaller bone spurs on the toes can be removed with a small incision and a burr power. Sometimes a tight tendon can be released through a very small incision. There are some innovative new systems and medical instrument companies that are coming up with techniques to do some procedures through a small incision. The following is an example of minimal incision surgery to remove a spur on the fifth toe. There is a before and after image of the x-ray. The incision on this is typically only 4 mm in length.