dr timothy young
Displaying items by tag: dr timothy young
Dr Timothy Young Discusses Bunion Surgeries

Dr Timothy Young Discusses Bunion Surgeries in Detail, Part 1
Bunion surgery is a common procedure performed by Dr Timothy Young and other Foot Surgeons to correct a bunion deformity. A bunion is usually combination of the first metatarsal being out of alignment and bony bump that forms on the joint at the base of the big toe. This can cause pain and discomfort when walking or wearing shoes. The bunion correction surgery itself usually takes 1-2 hours. The surgeon’s preparation for bunion surgery requires planning ahead and, requires attention to detail. In this blog, we will go over the steps that Dr. Young and other foot surgeons take to prepare for the best bunion treatment and the best bunion surgery.
Patient Evaluation
Before any bunion surgery, Dr. Young will evaluate the patient's medical history, medications, and overall health to make sure that our patients are good surgical candidates. Dr. Young will also examine the patient's foot to determine the severity of the bunion, the extent of the deformity, and the type of bunion surgery that would be most appropriate. For example, some patients have a severe bunion deformity and require a Lapidus or Lapiplasty procedure. Some patients have extreme adaptation of the great toe joint and require a procedure that realigns the joint. Some bunions are mild and yet the joint is not flexible and for this, decompressing the joint is an effective treatment. These evaluations come from both physically examining the foot, and imaging evaluation.
Imaging Tests
The surgeon will typically order imaging tests such as X-rays, CT scans, or MRI scans to get a better understanding of the bunion’s structure and position. This information will help the surgeon plan the surgery and determine the best approach to correcting the deformity. Dr. Young uses digital x-rays which allow for precise measurements and preoperative planning that can be done right on the computer.
Anesthesia Planning
Dr. Young will discuss the anesthesia options before surgery. Dr. Young often utilizes local anesthetic combined with MAC anesthesia (monitored anesthesia with conscious sedation). Other options include general anesthesia, regional anesthesia, or local anesthesia. The type of anesthesia can be discussed prior to surgery and will depend upon the patient's medical history and the type of foot surgery and the extent of bunion surgery. With MAC anesthesia combined with local anesthetic, the patient is still conscious and breathing on their own (not intubated). This is more like a twilight sleep and the patient's recovery extremely fast, and we can avoid the typical side effects that can be encountered with the general anesthetic.
The preoperative visit:
Dr. Young's patients come in the week prior to surgery to help them prepare for surgery. We will discuss details of the surgery itself and how to care for the foot after bunion surgery and if crutches or a special boot will be required. Also, the patient's medical history and medications are reviewed. Some medications will be avoided prior to surgery. Usually, the patient will be required to fast prior to surgery and need to make driving arrangements after the procedure. Our patients are given a special antibacterial scrub to do at home prior to surgery.
If you are experiencing foor or ankle pain, give us a call at 425-391-8666 or make an appointment online.
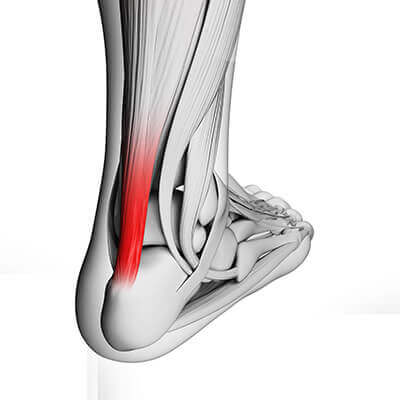
Dr. Timothy Young, a Board-Certified Foot Surgeon Discusses Tendinosis
The most effective treatments for this include prescription orthotics to address the mechanics and to reduce the mechanical shearing within the tendon. Calf stretching and a night splint can be very effective. KT tape is a useful adjunct for this problem. Shockwave therapy is extremely helpful for this condition. Some individuals will require surgery for this. This can involve removing some of the damaged portion of the tendon, and it can also involve lengthening the tight calf muscle with the gastrocnemius recession.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Plantar Verruca and Porokeratosis
Typically, this skin infection develops additional blood vessels through a process called angiogenesis. Therefore, it is classic for plantar verruca have multiple punctate or pinpoint patches of dried blood or eschar, and during the examination when we lightly remove the superficial layer of the verruca and callused area, we see pinpoint bleeding. This pinpoint bleeding is very helpful to accurately diagnose these as plantar verrucae. There is a similar appearing lesion that is often called a porokeratosis.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
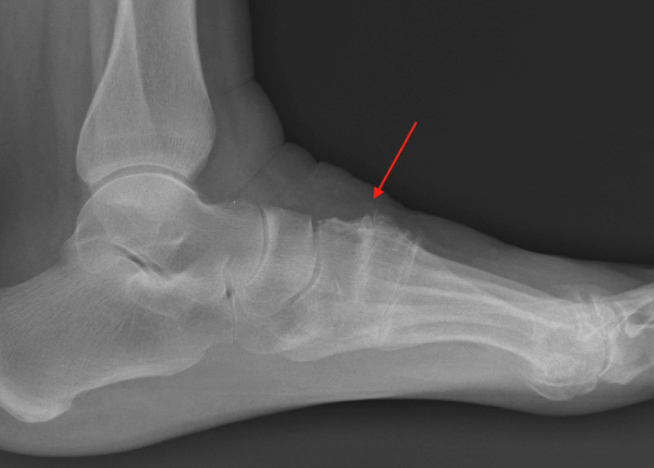
Dr. Timothy Young, a Board Certified Foot Surgeon Discusses Sesamoid Problems – Part 2

Dr. Timothy Young, a Board Certified Foot Surgeon Discusses Sesamoid Problems – Part 2
Problems with the sesamoid bones in the foot can be an overuse injury. As mentioned previously, some sports have higher association of sesamoid problems, such as dance. The injury and damage to the bones can range from inflammation of the soft tissue around the sesamoid bone and capsule. We call this sesamoiditis. Further damage could lead to fracture of the bones and this is often readily seen on an x-ray. The problem is that some individuals have sesamoids that, are as 2 separate bones or portions from birth (congenitally)
Therefore, it can be difficult to determine if it is a fracture or if it is a structural congenital condition. This is called a bipartite sesamoid when it is a congenital structural condition with 2 separate bones. Additional problems may include damage to the blood supply of the bone or avascular necrosis. This can be difficult to diagnose and often requires an MRI. A typical office based examination would include x-ray evaluation of the sesamoid bones. As mentioned this can clearly diagnose many fractures or arthritic conditions of the sesamoid bones. More subtle changes can be seen with ultrasound imaging. And as mentioned, an MRI is very useful for sesamoiditis especially if there is concern over potential avascular necrosis.
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online today.
Dr. Timothy Young - a Board Certified Foot Surgeon Discusses Sesamoid Problems – Part 1
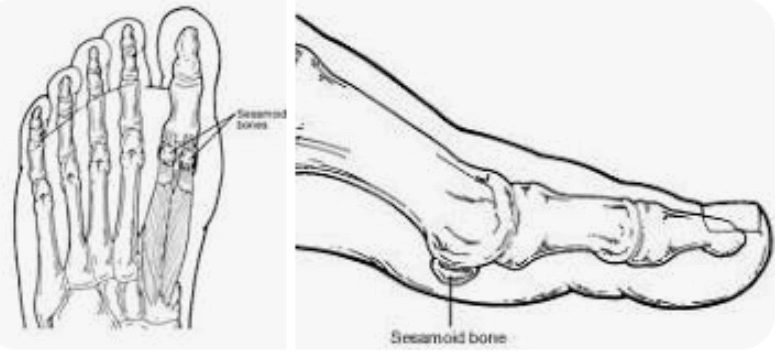
Dr. Timothy Young - a Board Certified Foot Surgeon Discusses Sesamoid Problems – Part 1
Sesamoid problems are fairly common in the feet. There are 2 sesamoid bones at the base of the great toe joint. These are small bones about the size of a pea. A larger sesamoid bone is the patellar kneecap. By definition, a sesamoid bone has a muscle and then the sesamoid bone which crosses the joint, and then there is a tendon from the sesamoid bone crossing over the joint to attach to the other side of the joint. In the knee, there is the quadricep muscle which attaches to the patella or kneecap, and then the knee Is attached to the tibia by the patellar tendon.
This muscle sesamoid bone and tendon complex crosses the joint and gives leverage and protection to the mechanical function of the joint. In the foot, the sesamoid bone can be very vulnerable. As soon as the heel comes up off the ground during gait and other full weightbearing activities, the load and weight is transferred to the forefoot and up to have to wait or more will be transmitted through the sesamoid bones into the head of the first metatarsal. Therefore, any running activity our other sports such as dance puts a heavy load on the sesamoid bones. These are common activities with the sesamoid bones can be injured or damaged.
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr. Timothy Young, a Board Certified Foot Surgeon, Discusses Treating Midfoot Arthritis
Dr. Timothy Young a board certified foot surgeon, discusses treating midfoot arthritis.
This can be a difficult access or find the correct entry point, therefore we use ultrasound guidance to verify correct placement of the synthetic join lubricant. There is some communication between these adjacent midfoot articulations or joints and therefore there is additional benefit by injecting the second metatarsal–cuneiform joint to some of the adjacent communicating joints. We typically use Supartz which is a highly purified form of hyaluronic acid. I typically use the same protocol for other joints such as the ankle joint which is a series of injections at 1 to 2 week intervals usually 3 to 5 injections.
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, a Board Certified Foot Surgeon, Discusses Supartz Injections for Ankle Arthritis
Dr. Timothy Young, A Board Certified Foot Surgeon, Discusses Postsurgical Scar Formation and Supplements

Dr. Timothy Young, A Board Certified Foot Surgeon, discusses postsurgical scar formation and supplements.
In addition after bone is resected bone often has excellent blood flow and there can be a blood clot or hematoma on the surface of the bone, deep within the wound. This can be resorbed by the body and also can eventually convert to scar tissue and again cause ongoing swelling or stiffness to the surgical site. Two supplements may be helpful for this. One is nattokinase and the other is serrapeptase. Both of these supplements should be taken 30 minutes before food for best absorption. The nattokinase can be taken once a day and this serrapeptase can be taken twice a day. Talk to your surgeon or naturopath to further discuss the role of these supplements with your particular situation.
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment online today.
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Neuroma Treatments
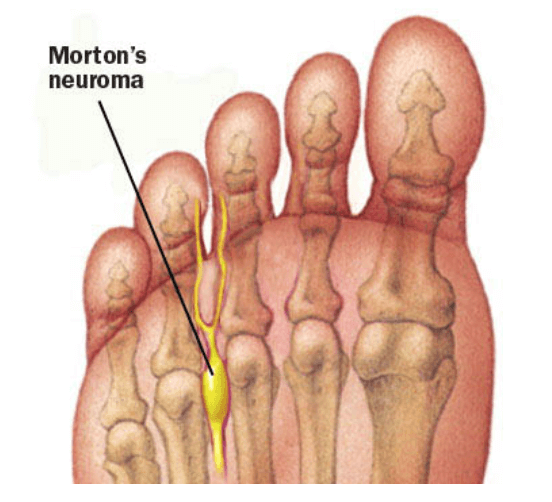
Dr. Timothy Young, a board-certified foot surgeon, discusses neuroma treatments:
Our Doctors have been using Alcohol injections for Morton's Neuroma for over 10 years with excellent success. Most patients have between 6 - 8 injections at weekly intervals. Occasionally a "mini-series" will be done after 12 months. For most patients, there is minimal discomfort after the injections and there is progressive relief from the Neuroma symptoms.
We typically use between 20-30% dehydrated alcohol. Ultrasound guidance is critical for correct injection technique. Most frequently we treat the 3rd intermetatarsal space, and runner up is the 2nd intermetatarsal space. This provides an excellent alternative to surgical treatment, and we also treat stump neuroma problems (where there is reoccurrence of the neuroma symptoms after prior foot surgery).
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr. Timothy Young, a Board-Certified Foot Surgeon, Discusses Evaluation of Bone Healing Status

Dr. Timothy Young, a board-certified foot surgeon, discusses evaluation of bone healing status.
How does your surgeon know when bone healing is adequate for unprotected weight-bearing for example if you have had bunion surgery and the bones were cut (osteotomy), then it’s important to stay in a protected boot or surgical shoe until there’s adequate bone healing. Typical bone healing takes approximately eight weeks for a healthy adult that can be less for young adult or teenager. X-rays can be helpful. A CT scan also can be helpful but can be quite expensive and often has artifact due to retained hardware causing magnetic interference with the imaging. One additional tool that I like to utilize is ultrasound imaging.
Ultrasound imaging can show subtle areas of bone bridging that you cannot see with a conventional radiograph. X-ray findings often lag behind the actual bone healing status. So, determining bone healing is always a challenge and based on a number of different indications such as age and health of the patient, appearance of x-rays, and post operative time frames. Oftentimes I can get a better assessment of the actual bone healing by utilizing ultrasound imaging. This often allows me to have our patients get out of their boot or cast earlier and then if I had to rely on x-rays alone.
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.