dr brandon nelson
Displaying items by tag: dr brandon nelson
Dr Brandon Nelson, A Board Certified Foot & Ankle Physician & Surgeon, Discusses Achilles Tendon Pain
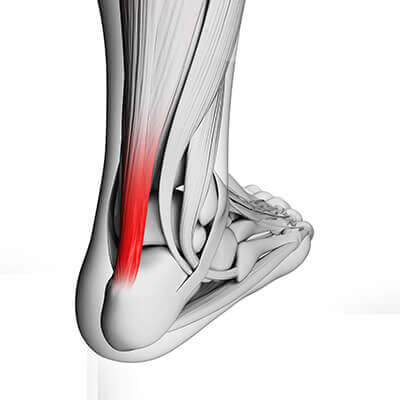
If you are an athlete at some point you have probably experienced Achilles tendon pain. Most people will have this type of ankle pathology after starting a new program or ramping up their current workout schedule. I personally have dealt with some insertional Achilles tendon pain and will give some insight as to what can be done to get you back to full speed.
It is important to know that the Achilles tendon is the biggest, thickest and strongest tendon in the human body. It has more pressure per square inch than any other tendon and is constantly under load and tension. Every time you step the Achilles tendon fires so it rarely has an opportunity to relax. This is the primary reason it is common to have tendonitis in this location.
Other factors contributing to this can be related to training issues or foot structure issues. Training issues are usually related to plunging into new techniques or training to hard. It is important to build up to new levels and allow adequate recovery to prevent tendonitis. I also am a big proponent of stretching and icing as this can speed recovery. Foot structure or anatomical design can also have a role in this pathology. Oftentimes patients will have a tight calf that they were born with. It is important to establish a stretching protocol that encourages at a minimum of 3 times a day. Other foot structures that cause Achilles issues are high arched feet or the cavus foot. These type of feet tend to overload the Achilles.
If you are suffering from Achilles tendon pain I can help get you back to full speed. Give us a call today at 425-391-8666 or make an appointment online.
Sincerely,
Board Certified Foot & Ankle Physician and Surgeon
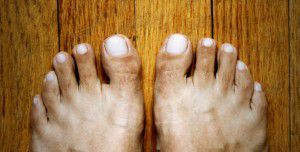
Dr Brandon Nelson, A Board-Certified Foot & Ankle Surgeon, Discusses Bunion Surgery

Bunions can become quite painful and make walking or exercising difficult. Additionally, shoe gear can become increasingly hard to find as the foot begins to widen. Most bunions are genetic in origin, however shoe gear and increased pressure can cause an acceleration of their growth. It will usually get to a point where one needs to consult a bunion expert and come up with a management plan. I normally consult on more than a few bunions per week and can help patients make decisions with what would be best with there current situation.
Conservative care may be an option for some people. I have taken over 10 years and developed a protocol that can provide significant pain relief and help slow the progression of a bunion. I typically will start with an x-ray and then go through all the options available for an individual patient. Even if you have seen another physician, it can be quite helpful to have a second opinion.
Surgery is also an option that can work very well for some people. I believe the most important step in this process is what a patient’s goals are. It is important to note the only way a bunion can be reduced in size is surgical. There are many different surgical options, and I will always take you through what is most appropriate in your circumstances.
If you have a bunion and would like a consultation, please call and schedule one today. I look forward to helping you.
Sincerely,
Board Certified Foot & Ankle Surgeon and Physician
Dr. Brandon Nelson, Board-Certified Foot and Ankle Surgeon, Discusses 3-D Bunion Correction

Bunions are by far the most common surgical procedure I perform. At this point in my career after practicing more than 10 years, I have performed thousands of bunion procedures. Bunion surgery itself is a highly successful procedure that has great outcomes and patient satisfaction.
The 3-D bunion correction or lapiplasty is a great tool that has accelerated the bunion surgery techniques. I find the procedure itself can be easily reproducible and has great long-term success. This is a great tool for large bunions and for patients that have had long-standing bunion deformities. It is important to see somebody but has experience performing this technique, because there are some technical challenges.
The Lapidus or lapiplasty is a most common bunion procedure I perform and I have found it to be extremely powerful surgical tool. If you have a long-standing bunion deformity and have had pain and irritation and are contemplating surgical reconstruction please make an appointment. I will happily review your x-rays and possible surgical options.
Sincerely,
Board-certified Foot and Ankle Physician and Surgeon
Dr. Brandon Nelson, Board-Certified Foot and Ankle Physician and Surgeon, Discusses Minimally Invasive Bunion Surgery

Bunion surgery has progressed significantly since its inception. Years ago, it was not uncommon for patients to stay overnight in the hospital if they had bunion surgery. Often times patients would spend days in the hospital and be in a cast and nonweightbearing for months. However this is a very rare occurrence these days and the majority of procedures are performed in an outpatient setting and very rarely is there an extended period of nonweightbearing. This evolution of bunion surgery has allowed for minimally invasive surgeries to become more commonplace.
Minimally invasive refers to making significantly smaller incisions than we’ll we typically do for bunion surgery. The average bunion can now be performed with minimally invasive surgery through an approximate 2 cm incision. The advantages of minimally invasive surgery is it allows for a quicker recovery and increased healing capacity. The majority of people will heal more quickly than the traditional open bunion procedure and will have less pain.
It is important to note that not every patient is a candidate for minimally invasive bunion surgery as it depends on other factors including overall foot structure and size of the bunion. It is important to have a thorough evaluation and workup for considering bunion surgery, any type of bunion surgery including minimally invasive. If you’re having bunion pain please contact my office and we will be able to get to an appointment and have your bunion evaluated. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Board-certified Foot and Ankle Physician and Surgeon
Dr. Brandon Nelson, Board-Certified Foot and Ankle Surgeon discusses Minimally Invasive Bunion Surgery

A bunion is a common forefoot condition that can be characterized by mild, moderate or severe and defined as a deviation of the big toe in the lateral direction. This condition is progressive and can lead to pain and discomfort with walking and exercise. Conservative measures are not usually successful. The traditional approach consists of an open incision and dissection of the foot that involves balancing of soft tissues and bony deformities. The procedure itself is highly successful but there is question as to whether more minimally invasive type accessible.
Minimally invasive bunion surgery has been around for years and as this technique is getting better, this becomes more of a promising type procedure. The literature is full of different types of minimally invasive bunion surgeries that can be used correct the foot. Some of the most promising new or techniques utilize screw or pin fixation and has become highly successful.
All done under direct live x-ray and results have been extremely positive. Majority of patients are weightbearing immediately after surgery and can return to normal shoes in 3-4 weeks. This is because of the soft tissues had minimal interruption and vascularity preserved. Minimally invasive bunion surgery shows promising results and can provide a fast return to activities.
If you’re suffering from bunion deformity and would like to discuss minimally invasive bunion procedure, call 425- 391-8666 or make an appointment online today.
Sincerely,
Dr. Brandon Nelson
Board-certified Foot and Ankle Physician and Surgeon
Dr. Brandon Nelson, Board-Certified Foot and Ankle Physician, Talks About Ingrown Nails
Ingrown nails can be extremely uncomfortable. They are caused from a bacterial infection typically in the big toe. Often times patients will have a history of ingrown toenails or family history of ingrown toenails. It is important to not try and treat ingrown toenails at home as this typically will make the infection worse. Ingrown nails themselves typically present as pain and swelling along the border of the toenail where the skin, patients will experience some drainage from the site and is often painful at times.
I recommend patients are evaluated when their nails are sore, red, thickened or painful with walking. There are many different options for treating an ingrown nail however typically the offending nail border has to be removed. Once removal is performed the procedure of choice is really dictated by the number of ingrown toenails the patient has experienced. The two options are an incision and drainage or what is called a matrixectomy.
Option one or incision and drainage involves removal of the offending nail border. This is typically done on just the side that is painful. Prior to removal the toe is anesthetized, cleaned and sterile prep. Nail is then removed with the hemostat appendicitis, flushed and covered with a sterile compressive dressing. Typical recovery from something like this is patients can return to activities the next day or so once a day for 1 week.
A matrixectomy involves a similar technique as described above. However once the nail is removed the nail cells are cauterized to prevent them from growing back. Matrixectomy is a procedure specifically designed for someone that has a history of recurrent ingrown toenails or long family history of ingrown nails. The patient’s toe will be red and sore often times for 2-3 weeks after the procedure.
If you’re experiencing painful swollen digit please give me a call today and I can help 425-391-8666, or make an appointment online.
Sincerely,
Board-Certified Foot and Ankle Physician and Surgeon
Dr. Brandon Nelson, Board-Certified Foot and Ankle Physician and Surgeon, Discusses Outcomes for Bunion Surgery

Bunion surgery continues to be the most common foot and ankle surgery performed and there are many different procedures available. Not all of the procedures have equal outcomes. The most common bunionectomy performed in the United States continues to be what is called an Austin bunionectomy or a head procedure. This type of procedure is primarily used to correct mild to moderate bunions. This procedure has great outcomes, as patients do well ambulatorily postoperatively. Most patients will be back to activities fairly quickly and long-term results are good as long as there are no other foot deformities. This type of bunion procedure is fairly straightforward and can be performed in 30-45 minutes. Postoperative protocol is easy and pain level is generally mildly and well controlled with oral medications.
The second most common type of bunionectomies are for severe bunions or people with foot instability. These procedures usually involve more in depth bunionectomy or stability type procedures. The most common bunionectomy for this is what is called a Lapidus bunionectomy. This procedure involves fusion of bones on the inside of the foot and provides great correction and increased stability for the foot itself. This procedure can often involve a period of nonweightbearing or modified weightbearing and usually takes longer to heal from within the previously discusses bunion. However it should be noted the recurrence rate with this type of bunionectomy is much less and the long-term outcomes are are great. Again, it is important to address other foot structure issues as these can have effect on long-term results.
If you’re suffering from a bunion or foot pain, an evaluation is essential. Call the office at 425-391-8666 or make an appointment online today so I can help.
Sincerely,
Board-Certified Foot and Ankle Physician and Surgeon
Dr. Brandon Nelson a Board Certified Physician & Surgeon Discusses How Heel Pain Can Be Fixed Permanently

The most common cause of heel pain continues to be plantar fasciitis in adults and apophysitis (or Sever’s Disease) in children. With adults it seems to be correlated with an increase in exercise or activities and with children it is common with growth spurts. The two conditions often have similar presentations and can be treated with similar protocols. I recommend having any pain evaluated by a physician as other pathologies can cause heel pain.
They are many different treatment options for heel pain, especially plantar fasciitis. I have now observed different conservative and surgical techniques come in and out of favor. It is important to first get the correct diagnosis and then see what factors are contributing to the pain before implementing treatment. It can be helpful to have and x-ray, an ultrasound or even an MRI before tackling heel pain.
In recent years I have began to approach plantar fasciitis from both a mechanical and biological perspective. I believe foot structure and training can play a large part in the development of heel pain. I also believe once this heel pain starts it often can become chronic and this chronicity is what allows the pain to spiral out of control. Since implementing a protocol that addresses both of these aspects I have seen a huge swing in long term effectiveness. If you are suffering from heel pain for months or even years I can help you fix this once and for all. I know how painful, frustrating and exhausting it can be.
Board Certified Physician and Surgeon
Dr Brandon Nelson, a Board-Certified Physician and Surgeon, Discusses What His Patients Experience After Bunion Surgery

I have now been operating for about 15 years and can tell you bunion surgery has really changed. In the average week I correct 3-5 bunions and have now operated on 1000’s of bunions. Some bunions are small, and some are large and very complex, but all can be fixed. I continue to learn and research new techniques, and these have afforded me opportunities and skills to provide great outcomes and minimal down time.
In the past bunion surgery was done at the hospital and often required and overnight stay. Patients were placed in casts and often non-weight bearing for months. I have heard stories of patients being uncomfortable for weeks.
I can tell you techniques have changed, and I am happy to outline how the average patient experience goes at my clinic. My clinic has an onsite surgery center that provides a huge cost and time savings as compared to a free-standing surgery center or a hospital. Most bunion cases are completed in under 3 hours from the time one enters the clinic to when ones leaves. We utilize IV sedation which is safer and allows me to perform a nerve block for long term pain relief. Pain medication is only needed for a few days and many patients do not even take anything apart from an NSAID. Weight bearing status depends on any ancillary procedures, but most bunion patients can walk immediately after surgery.
If you have bunion and have been contemplating having it fixed make an appointment today and I will review your options and help you make an informed decision.
Sincerely,
Dr Brandon Nelson, A Board-Certified Physician and Surgeon, Discusses Options to Treat Neuromas
Neuromas of the foot are common in woman between the ages of 40-60. The typical neuroma will present with pain, burning and tingling to the forefoot. Most people state the pain feels better without shoes and rubbing one’s foot can help. There does not need to be a history or trauma or even previous foot pain to have a neuroma.
The neuroma itself is usually located in the 3rd interspace of the foot. This is between the 3rd and 4th toe and can be either right or left foot and rarely both feet. The reason this is the most common spot is the fact two nerves come together in this location. Often this creates an entrapment as this location can have limited space.
Treatment options for neuromas range from stretching and icing to injections and orthotics. Rarely now is surgery required as the conservative measures are so successful. I typically employ a prescription orthotic in conjunction with a series of alcohol injections. I have developed a protocol over years of treating thousand of patients and this has proved so successful that I rarely find surgery needed. I even see quite a few patients that have seen multiple other providers. If you want to avoid surgery and have a neuroma I can help. I look forward to getting you back on the road to recovery, Dr. Brandon Nelson, Board Certified Physician and Surgeon.
Give us a call at 425-391-8666 or make an appointment online today.