podiatrist issaquah
Displaying items by tag: podiatrist issaquah
Dr. Timothy Young, a Board Certified Foot Surgeon, Discusses How to Tell if a Fracture is Healing
If you are experiencing foot or ankle pain, give us a call at 425-391-8666 or make an appointment onine today.
Mid Foot Bone Spurs and Surgery Part Two
Mid foot bone spurs and surgery part two.
Surgery to treat a bony prominence in this area usually is very straightforward. It typically involves an incision directly adjacent to the prominence or bone spur. We surgically go down to the tissue layers and then expose the bony prominence. Then most commonly a power burr is used to smooth down the excessive bone in the area or sometimes a special surgical saw. The wound is cleaned up and flushed to remove any small bone fragments.
The remaining cut bony surface usually has an excellent blood supply and can cause swelling problems or even a small collection of blood like a hematoma. Therefore several different techniques can help deal with this. One is to use a small drain which allows for a path for the blood to escape the area, this is especially useful for the first several days postop. Another strategy is to use bone wax to seal the bone.
Some Surgeons use topical fibrin to help clot exposed bleeding vessels that are small and embedded in the bone. After the bone remodeling procedure is done, the soft tissue layers are closed and the procedure is then complete. Usually it’s a relatively quick recovery. Remember that we are talking about a bony prominence without significant underlying midfoot arthritis. The midfoot arthritis and surgical fusion of the involved joint can be a longer recovery.
If you have questions about spurs or bumps on the top of your feet forefoot surgery in general, and would like a consultation please let us know. Give us a call at 425-391-8666 or make an appointment online.
Dr. Brandon Nelson, A Board Certified Physician, Discusses Burning and Tingling In The Foot
What is it?
Burning or tingling can be one of the most challenging symptoms to treat in the foot. The number one reason patients have burning of tingling in the foot is neuropathy. Neuropathy is a disfunction of the sensory nerves in the lower extremity. The most common cause for neuropathy is diabetes. High levels of glucose in the body can attack the nerves and lead to burning and tingling. There are other causes including medications, alcoholism and exposure to toxic metals. Additionally, about 60% of neuropathy is idiopathic, meaning we are unable to identify a cause. Neuropathy typically gets worse as time goes on and can become quite debilitating for patients.
How can we help?
We understand how frustrating neuropathy can be and how emotionally taxing it can become. Our goal is to help identify the cause and to help decrease the factors that make it worse. We have now established a protocol that significantly reduces the symptoms of neuropathy. Recently I had a patient tell me he felt his feet for the first time in 10 years. We have a combination approach that is extremely successful. We utilize an FDA approved laser for neuropathy in combination with some vitamin supplements that are specifically designed for nerve pain.
If you are suffering from neuropathy or fibromyalgia we can help, schedule an appointment today. Give us a call at 425-391-8666 or make an appointment online.
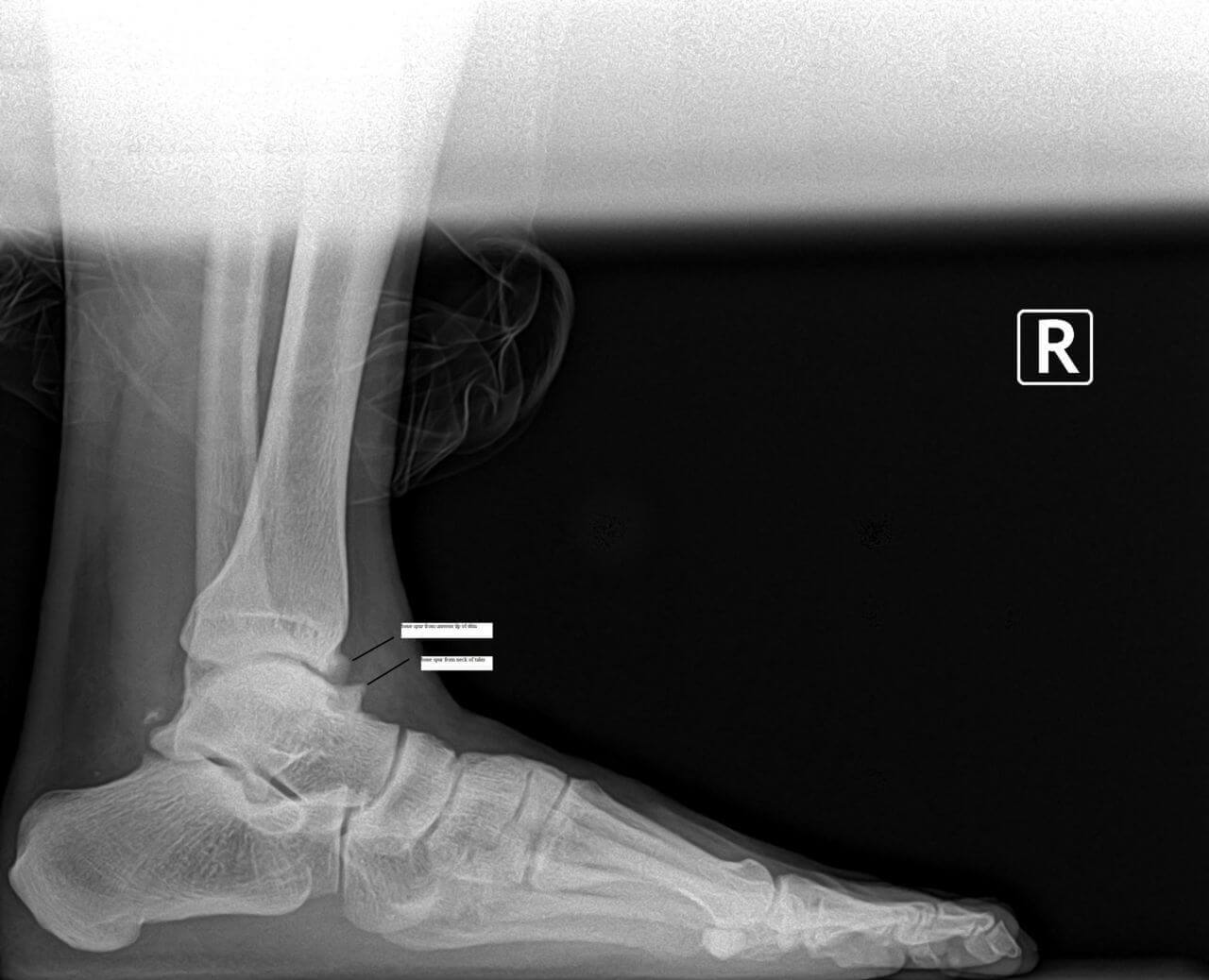
Dr. Brandon Nelson, a Board Certified Physician, Discusses Achilles Tendonitis
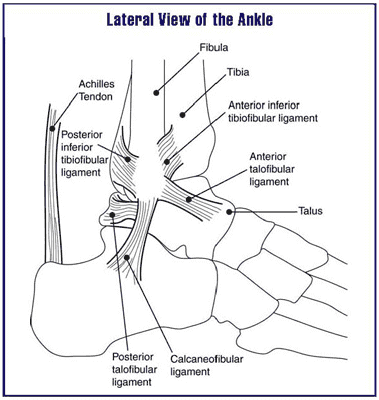
The Achilles tendon is the work horse of the lower extremity. It provides forward propulsion and is the thickest, strongest tendon in the human body. It basically never has a chance to rest if you are walking. The tendon itself is made of three different muscles and contracts to provide power. That is why it is one of the most common tendons to experience tendonitis in.
It is probably the most common type of tendonitis we see in the office. I would also say it is one of the most challenging to treat. The challenge is it's constantly in use and the number one cause of Achilles tendonitis is overuse. We see a fair amount as the summer starts and people get outside. The other big culprit is a new exercise program. Most of these patients are usually men and around the age of 40.
I encourage patients to get in early and treat this aggressively. The Achilles tendon is notorious for taking a long time to return to a normal state and recover from tendonitis. The earlier and more aggressive the treatment the better the long-term outcomes. Focusing on eliminating the abnormal pull of the Achilles and stretching provide relief. There are numerous opportunities to administer more advanced treatment options that utilize the body's own ability to heal. These techniques seem to have the best long term outcomes. If you are suffering from Achilles’ tendon pain we can help.
Give us a call at 425-391-8666 or make an appointment online today.
Dr. Brandon Nelson, A Board Certified Physician, Discusses Metatarsalgia And Foot Filler For Fat Pad Atrophy
Metatarsalgia refers to pain and inflammation under the metatarsal heads in the foot. Patients often experience burning or tingling or even bruised type sensations in the ball of the foot with walking and exercise. This is often caused by the lose of fat pad or cushioning in the foot. This can occur as a normal aging process or as a genetic predisposition.
One of the best options available to treat fat pad atrophy or loss of fat pad or metatarsalgia are foot fillers. These foot fillers can be used to replace natural cushioning in the foot. There are many different types of foot fillers. I prefer to use adipose tissue as it is a naturally occurring product and provides no immune response. Adipose transplant can be highly effective long term and can be preformed in the office with local anesthetic. Most people find significant relief for long periods and have very little down time.
If you have metatarsalgia or loss of fat pad, contact my office today and request a consultation.
Give us a call at 425-391-8666 or make an appointment online today.
Dr. Brandon Nelson, a Board Certified Bunion Expert, Discusses How to Treat Your Bunion Non-Surgically
.jpeg)
Bunions can be very challenging for patients, especially if you are active and enjoy activities like hiking and running. The bunion itself is primarily an inherited foot structure issue that gets worse with time. I think that is a good point to revisit. The only way to stop your bunion from increasing with time is to stop walking. I say that to highlight the fact your bunion will get bigger, however the rate of development can be slowed or even fixed. There are many options for conservative measures and I will discuss a few.
Bigger and wider shoes, this is probably the most common measure. Buying your shoes like this will allow more room for the bunion and often alleviate some of the pressure issues. However, this does nothing to treat or even slow down the bunion.
Stretching, splinting, toe spacers, straps that are all over the internet and shoe stores. These do absolutely nothing to prevent or reverse your bunion. There are quite a few variations on these, but if your bunion could be fixed with a strap or padding we would never have the need to operate on a bunion. The main thing to remember this is a bone deformity, a mal-alignment of bones that is inherited. The bunion itself gets bigger when you place pressure on it. Strapping and toe spacers do sometimes provide a little bit of soft tissue stretching that can temporarily make your pain less.
Over the counter inserts, again not much help. Your feet are unique to you and the position of your bones are usually not in the correct place with a bunion. The best option here is to go with a custom molded prescription orthotic. Our clinic has worked with a local lab to develop a bunion specific orthotic that can actually slow down the development of your bunion. Do not waste your money on an over the counter, even the inserts that are molded to your foot are not enough.
If you have bunion pain, make an appointment today so we can help you slow your bunion growth and eliminate the pain.
Dr. Brandon Nelson, A Board Certified Foot & Ankle Physician, Discusses Heel Pain

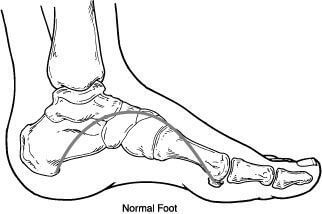
Heel pain has a variety of causes and can be challenging for many patients. Most patients with heel pain describe it as a dull ache, or a bruised sensation but some have tingling and burning. The main causes of heel pain are plantar fasciits, bursitis and nerve entrapments. Sometimes there are overlapping symptoms and some patients even have multiple causes.
Plantar fasciitis is by far the most common cause of heel pain. It presents as pain when you get out of bed, or first step pain and often gets a little better as the morning goes on. However, typically the pain returns every time you stop and sit and then get back up. Plantar fasciitis usually feel like a bruise to the bottom of the foot.
Bursitis, or bursal sack formation is usually found in people with a high arch. The bursa forms to help cushion the foot and is important in situations where a heavy heel strike occurs. Many times you can feel the soft bursa, or what seems to be a bubble under the heel.
Nerve pain and entrapments can occur do to anatomical constrictions in the foot or the ankle. These are often the hardest to diagnosis and can cause a myriad of symptoms. However, the most common are burning and tingling.
If you are suffering with heel pain we can help get you pain free. Heel pain is the most common pathology we see and are treatment protocols work quickly and effectively. Do not suffer for the summer make an appointment so we can help.
Give us a call at 425-391-8666 or make an appointment online today.
Bunion Surgery and Bunion Correctors, Dr. Brandon Nelson, a Board Certified Bunion Surgeon, Discusses Both
.jpg)
Bunions are a common pathology that presents to my practice. The majority of bunions are seen on women between the ages of 30-50. Most have noticed the bunion at an early age and slowly have noticed them grow. A lot of patients feel their shoe selection has contributed to the growth or their activities like running. We know that bunions are an inherited foot structure that gets worse with time and usage.
Bunion correctors are common on the internet and I have seen them all. What we know about bunion correctors are they can help relieve some pain that is related to soft tissue contractures. The bunion itself is a bony malalignment of the foot and the bunion corrector cannot move bone back into position. The bunion corrector can help stretch some of the soft tissues as the bunion gets larger. However, it should be noted no bunion split or corrector will fix you bunion or change the shape of your bunion.
Bunion surgery is the only way to realign the bones that cause a bunion. I recommend bunion surgery for anybody that is having pain or difficulty fitting shoes. I consult and hundreds of bunions a year and can tell you that they are not all the same. It is very important to have a complete workup including physical exam and x-ray of the bunion. Proper procedure selection is key to fixing the bunion correctly.
If you are experiencing bunion pain and would like a consultation please call us at 425-391-8666 or make an appointment online and I will review all your options from conservative to surgical at your appointment.
Dr. Brandon Nelson, A Board Certified Physician, Discusses Capsulitis of the Second Toe
Capsulitis is an inflammation of a capsule or joint. Your joints are defined by where two bones come together and have cartilage on the opposing surfaces and a joint sac (capsule) that encircles the two ends of those bones. Additionally in the joint capsule is fluid which helps the joint to glide smoothly.
The human body has many joints, the human foot has the highest concentration of joints with 33. The foot is an extremely complex structure and small deviations in the alignment can cause significant problems.
Capsulitis can have many causes, one of the most common is abnormal wear of a joint. Abnormal wear of a joint is usually attributed to increase pressures in that joint and can ultimately lead to arthritis. In the foot instability of the big toe can increase pressure in the 2nd toe leading to inflammation of that joint, the 2nd metatarsal phalangeal joint or MTPJ. What is typically seen is a patient with a bunion or a flat foot that causes results in high pressures of the 2nd MTPJ and the net result is pain. The pain can present with swelling, numbness or tingling. The eventual progression of this can lead to dislocation of the toe or what we call a cross over toe.
If you have pain around the second toe, icing and stretching can be very helpful. However it is important to have your foot evaluated as this is usually a progressive deformity that can cause increasing discomfort and eventual structural changes. I recommend an x-ray and an overall foot exam. Often times there are great conservative options to help this condition and help patients return back to activities. If you have 2nd MTPJ pain give us a call at 425-391-8666 or make an appointment online today.
Dr. Timothy Young a Board Certified Foot Surgeon, Talks About Capsulitis of the Second Toe and a Bunion Deformity Combined

This is a common combination.
When this happens in the first metatarsal does not carry its fair share of weight. It is common, for the next in line 2nd metatarsal to develop a stress overload. We can evaluation both conditions with an x-ray. We sometimes use an MRI to evaluation the extent of the 2nd toe capsulitis including for a capsular tear or plantar plate tear. Both the bunion and the 2nd toe capsulitis can be a difficult combination to treat.
The best bunion treatment can involve shoes and orthotics can also help with non-invasive bunion treatment. Bunion treatment options may be limited in severe cases and often need surgical treatment.



