bone spurs
Displaying items by tag: bone spurs
Dr. Timothy Young discusses a different kind of bone spur in the foot: Enthesophytes, not your typical bone spur.

Dr. Timothy Young discusses a different kind of bone spur in the foot: Enthesophytes, not your typical bone spur.
Introduction:
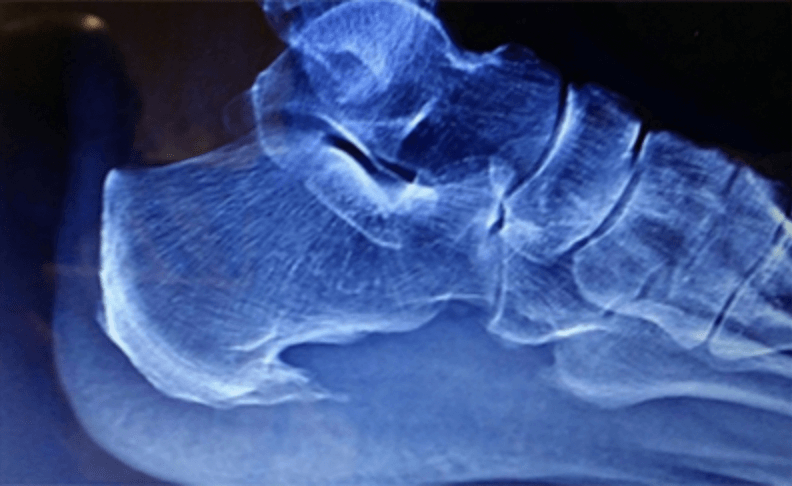
There can be confusion when talking about bone spurs in the foot. In general, when one thinks of an arthritic bone spur, that is often an osteophyte. However, there is a different kind of bone spur; this is an enthesophyte. The best way to think of an enthesophyte is calcification of the tendon or ligament at its attachment to the bone. A common example would be a heel spur related to plantar fasciitis or calcification of the Achilles tendon where it attaches to the back of the heel bone. It is important to know, however, that calcification of the Achilles tendon or a plantar calcaneal heel spur, in either case, may not cause any pain or symptoms at all. On the other hand, if there is associated inflammation or degenerative changes, there may be symptoms and pain.
Enthesopathy is another similar term describing this condition. Note that Enthesopathy often occurs in response to a mechanical condition, but there can be more of a systemic inflammatory condition also, such as ankylosing spondylitis or psoriatic arthritis. Some of the autoimmune arthritic conditions may potentially be related to this condition.
Enthesophytes vs. Osteophytes: An Overview
Enthesophytes Defined: Enthesophytes are abnormal bony projections that occur at the attachment points of tendons or ligaments to the bone. These bony outgrowths are the result of the body's response to chronic stress and irritation in these connective tissues.
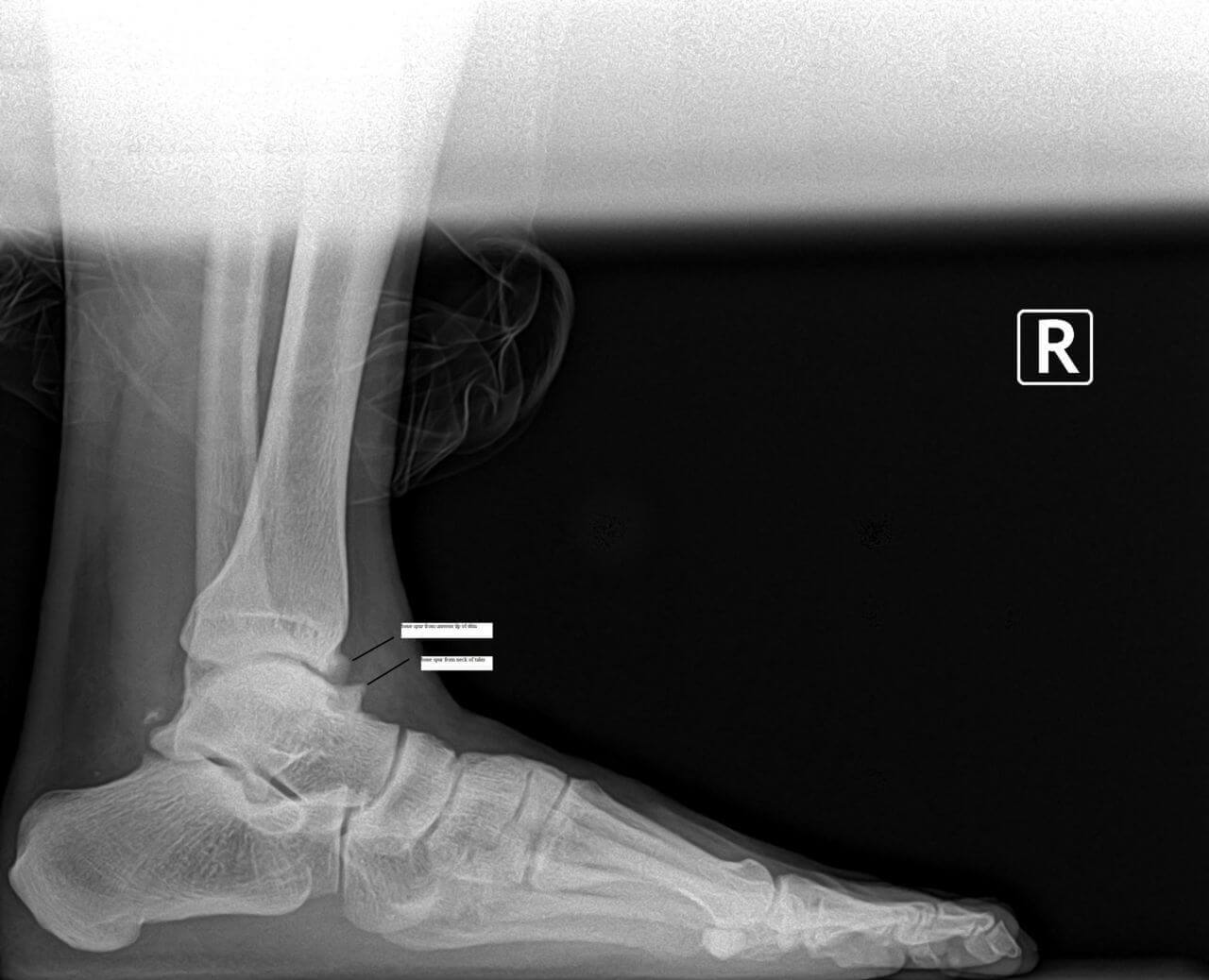
Osteophytes in Contrast: We have previously discussed osteophytes in our prior blog. Osteophytes are abnormal bony projections that form within joint spaces. Unlike enthesophytes, which are associated with the insertion points of tendons and ligaments, osteophytes develop as a response to joint degeneration and inflammation, often associated with conditions like osteoarthritis. The most common osteophytes in the foot and ankle could include the great toe joint, where bone spurs limit motion and cause an enlargement on the top of the joint. In the ankle, it is often the front of the ankle joint that develops osteophytes that can also limit ankle joint motion.
The Stress Response: Understanding Enthesophyte Formation
Chronic Tendon or Ligament Stress: Enthesophytes are born out of the repetitive stress and strain on tendons and ligaments. This stress can result from various factors, including overuse, improper biomechanics, or inflammatory conditions affecting the connective tissues.
Microtrauma and Inflammation: Microscopic damage to the tendon or ligament can lead to localized inflammation. As the body attempts to repair this damage, the bone responds by forming additional bony tissue at the insertion point – thus, an enthesophyte is born.
Common Locations: Enthesophytes can occur at multiple sites throughout the body. Common examples in the foot include the heel, with two common examples being Achilles enthesophyte and an enthesophyte associated with plantar fasciitis or the most typical heel spur.
Distinguishing Features: Enthesophytes vs. Osteophytes
Location:
Enthesophytes: Develop at the attachment sites of tendons or ligaments to bones.
Osteophytes: Form within joint spaces in response to joint degeneration.
Associations:
Enthesophytes: Linked to chronic tendon or ligament stress and inflammation.
Osteophytes: Associated with joint degeneration and conditions like osteoarthritis.
Clinical Manifestations:
Enthesophytes: May cause localized pain at the attachment sites, especially during movement.
Osteophytes: Can impact joint movement, causing pain, stiffness, and reduced range of motion.
Managing Enthesophytes: It is important to understand that in many cases, it is really because of the enthesopathy that we are treating so for calcification of the Achilles tendon, we often are treating Achilles tendon problems. And for treating a plantar calcaneal spur, we often are treating plantar fasciitis as the primary problem, and the enthesopathy may be a secondary problem.
Conservative Measures:
Rest, activity modification, and gradual return to exercise.
Physical Therapy: Stretching and strengthening exercises.
Anti-Inflammatory Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs) to manage inflammation and pain.
Orthotic Support:
Proper footwear and orthotic devices to alleviate stress on affected areas.
Shockwave Therapy: This is extremely effective at treating Achilles tendon problems and calcific Achilles insertional tendinosis and plantar fasciitis.
Platelet Treatments: Concentrated platelets are injected into the damaged tendon or plantar fascia.
Surgical Procedure Interventions:
Tenex: This is a less invasive type of procedure that can remove damaged tendon and remove some of the calcified portions.
Traditional Surgery: In resistant cases, surgical direct treatment may be considered.
Conclusion:
Enthesophytes may relate to the body's adaptation to the demands placed on tendons and ligaments. This condition may (or may not) cause discomfort, especially in the presence of chronic stress, and may limit exercise. Understanding their distinct nature and differentiating them from osteophytes is crucial for accurate diagnosis and effective management. If you suspect the presence of enthesophytes and experience persistent pain or discomfort, please contact our office for consultation or make an appointment online.
Dr. Timothy Young, a Board-certified Foot Surgeon discusses bone spurs in the foot: Osteophytes
Dr. Timothy Young, a Board-certified Foot Surgeon discusses bone spurs in the foot: Osteophytes
Defining Osteophytes: Osteophytes, a subset of bone spurs, are characterized by the outgrowth of new bone on the margins of a synovial joint. They often develop in response to joint degeneration and are associated with conditions like osteoarthritis.
Locations of Foot Osteophytes:
1. Joints: Osteophytes often form on the margins of joints of the foot, impacting movement and causing pain.
2. Edges of Bones: They may also develop along the edges of bones, affecting the alignment of joints.
Causes and Risk Factors:
1. Joint Degeneration: Osteoarthritis, a common cause of bone spurs, leads to the breakdown of cartilage and prompts the body to form osteophytes.
2. Repetitive Stress: Continuous mechanical stress on specific areas of the foot, often due to poor biomechanics or ill-fitting footwear, can contribute to the development of bone spurs. This often involves the force of gravity on weight-bearing joints. A good example would be the ankle joint.
Symptoms and Diagnosis:
1. Pain: Persistent pain in the affected area, especially during movement or weight-bearing activities.
2. Reduced Range of Motion: Difficulty moving the affected joint due to the presence of bone spurs.
3. Visible Bumps: In some cases, visible or palpable bumps may be present, indicating the presence of bone spurs. A good example this would be a bump on the top the midfoot that is due to large osteophytes in this location.
4. X-rays and ultrasound: x-rays and ultrasound can show the osteophytes. It is usually not necessary to do an MRI or CT scan.
Treatment Options:
1. Conservative Measures:
- Rest, ice, compression, and elevation (R.I.C.E.).
- Orthotic inserts and supportive footwear.
2. Physical Therapy:
- Stretching and strengthening exercises.
- Therapeutic modalities to alleviate pain and inflammation.
3. Medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain management.
4. Injections: injections can deliver medication such as Supartz which is a synthetic joint lubricant. This was originally FDA approved for the knee but is now used throughout the body. For the foot and ankle, it is most commonly used in the ankle joint and the great toe joint. Cortisone is not used as often, since repetitive use can weaken the existing Cartledge and adjacent joint capsule.
- In severe cases, surgical removal of the bone spur may be considered, or in some cases the joint can be stabilized by fusing it or placing an implant in the joint.
Conclusion:
Bone spurs and osteophytes in the foot can present challenges, but with proper understanding and timely intervention, individuals can manage their symptoms effectively. If you suspect the presence of bone spurs in your foot, please contact our clinic and we can review your options.
Mid Foot Bone Spurs and Surgery Part Two
Mid foot bone spurs and surgery part two.
Surgery to treat a bony prominence in this area usually is very straightforward. It typically involves an incision directly adjacent to the prominence or bone spur. We surgically go down to the tissue layers and then expose the bony prominence. Then most commonly a power burr is used to smooth down the excessive bone in the area or sometimes a special surgical saw. The wound is cleaned up and flushed to remove any small bone fragments.
The remaining cut bony surface usually has an excellent blood supply and can cause swelling problems or even a small collection of blood like a hematoma. Therefore several different techniques can help deal with this. One is to use a small drain which allows for a path for the blood to escape the area, this is especially useful for the first several days postop. Another strategy is to use bone wax to seal the bone.
Some Surgeons use topical fibrin to help clot exposed bleeding vessels that are small and embedded in the bone. After the bone remodeling procedure is done, the soft tissue layers are closed and the procedure is then complete. Usually it’s a relatively quick recovery. Remember that we are talking about a bony prominence without significant underlying midfoot arthritis. The midfoot arthritis and surgical fusion of the involved joint can be a longer recovery.
If you have questions about spurs or bumps on the top of your feet forefoot surgery in general, and would like a consultation please let us know. Give us a call at 425-391-8666 or make an appointment online.
Bone Spurs, Corns and Pressure Points on Your Toes
Dr. Timothy Young talks about removing a bone spur and corns and pressure points on your toes.
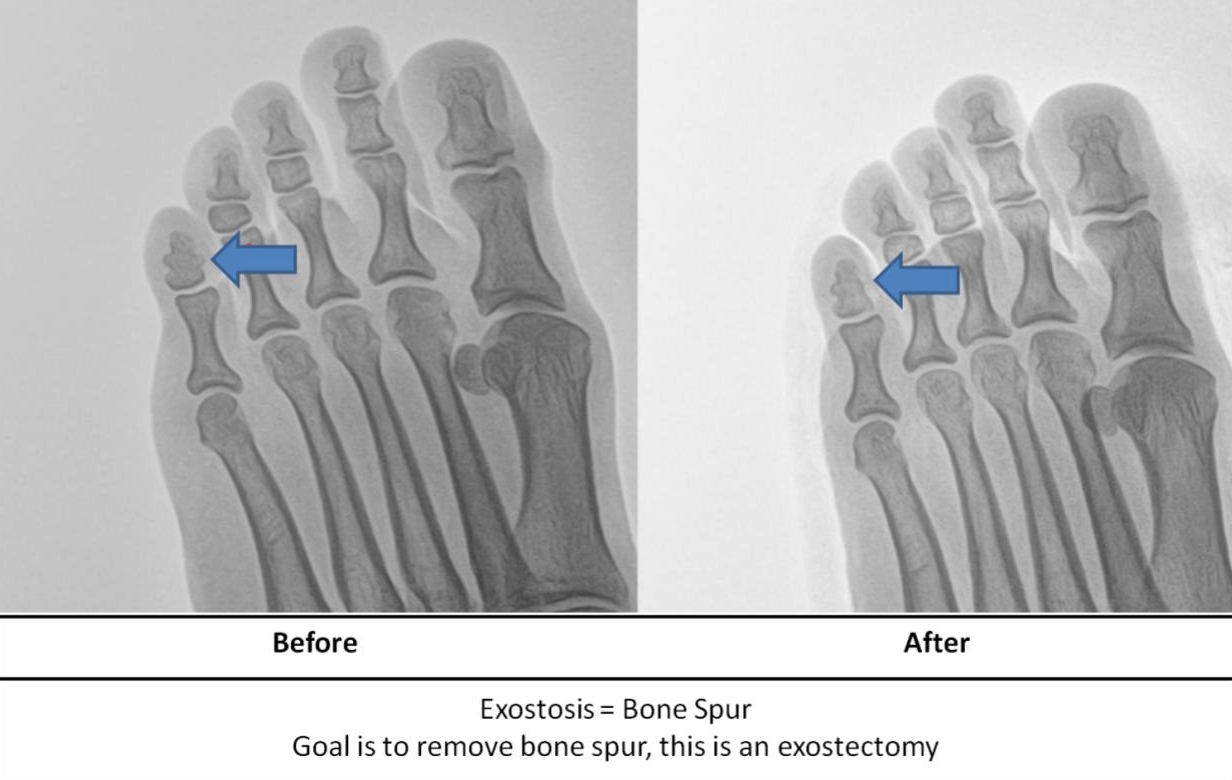
There are different types of bone spurs. Our focus today is on the 5th toe and problems when it overlaps the 4th toe. The inside or medial aspect of the 5th toe has a natural prominence where the medial condyle of the toe pushes against the adjacent side of the 4th toe. If this bone is enlarged we call it a bone spur or exostosis. This pressure point can become a red irritated patch of skin, or it can become a thickening of skin called a corn, or it can get so bad that the skin becomes an open wound.
Some of our patients are fortunate and roomier shoes or pads can alleviate the problem. Some of our patients just want the problem to go away and to have the bone spur removed.
The procedure to remove the bone spur is one of the easiest foot procedures we provide. Once the toe has local anesthetic, the procedure involves a tiny incision and then a special instrument is used to smooth down the bone enlargement. The site is flushed and a steristrip or a single suture can be used. A roomy shoe or surgical shoe can be used for a week and then use a gym shoe for another week and you are done. The recovery is very minimal and you are done. Problem solved. At Issaquah Foot and Ankle Specialists, we have an onsite surgical center that can save you time and money.
If you have a problem like this, please come in to discuss it with myself – Dr. Timothy Young, or my partner – Dr. Brandon Nelson.



