podiatrist issaquah
Displaying items by tag: podiatrist issaquah
Dr. Timothy Young, a Board Certified Foot Surgeon, Discusses How to Enhance Results of Hallux Limitus Surgery with a Cheilectomy
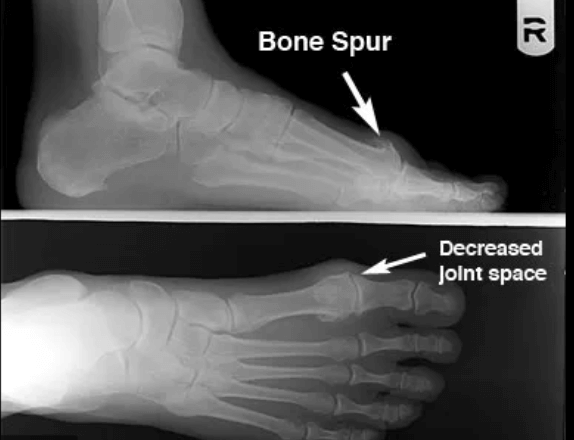
Dr. Timothy Young a board certified foot surgeon discusses how to enhance results of hallux limitus surgery with a cheilectomy.
If you have arthritis of your great toe joint or questions about potential surgery or procedures for this please request a consultation at our clinic. Give us a call today at 425-391-8666 or make an appointment online today.
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discuss Bunion Surgery

Bunion surgery is probably the most common procedure I execute. Most bunions can be fixed in about 2 hours and provide great long-term results. The most important factor is to have a thorough workup and x-rays to evaluate the foot. Once the foot and x-rays have been done then a plan for surgical or conservative care can be formulated.
If surgical intervention is called for, our office has an onsite surgery center which can save the average patient thousands of dollars as compared to free standing ASC’s or the Hospital. Our certified surgery center provides the best possible patient experience and has been functioning for over 15 years. If you have a bunion and have been contemplating what to do, I can help. I really enjoy helping people with bunions. Please make an appointment and we can discuss your options. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Lapiplasty Surgeon Dr. Brandon Nelson, Discusses 3-D Bunion Correction

The Lapiplasty technique has created an effective tool for bunion surgery. The foot and ankle surgeon community has seen a reproducible tool that has helped revolutionize bunion surgery. This procedure has helped bunion surgeons get the best possible correction with incredible long term outcomes. The Lapiplasty combines a tried-and-true bunion surgery technique with modern jigs and fixation. Bunion surgery is challenging and any tools that can help with getting better outcomes are looked upon favorably. This is the case for the Lapiplasty system.
As a Board-Certified Surgeon and Physician and somebody that has done 1000’s of bunion surgeries, this is a welcomed tool in my armamentarium. I have found that Lapiplasty is a game changer. I find my results are outstanding and long lasting. I look forward to helping more patients with bunion recover faster and returning earlier to activities is a giant plus! If you suffer from bunion pain come see if you are a candidate for Lapiplasty. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Dr. Timothy Young, a Board Certified Foot Surgeon, Discusses Collagen Supplements After Surgery
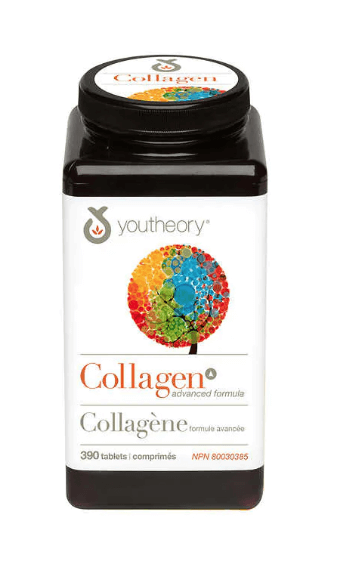
Dr. Timothy Young, a Board Certified foot surgeon, discusses collagen supplements after surgery.
For example Achilles tendon surgery or repair of an Achilles tendon rupture. Peroneal or posterior tibial tendon surgery. In addition zinc (25 mg up to 50 mg per day) and boron (3 mg per day) are supplements the can be helpful with deep tissue healing and wound healing. It's important to note that zinc can compete with some other essential elements such as calcium and magnesium so it's best to take zinc by itself for example at lunchtime. Remember there are always things that you can do to help your body heal.
If you are experiencing foot or ankle pain, please give us a call at 425-391-8666 or make an appointment online today.
Dr. Brandon Nelson, A Board-Certified Foot & Anke Surgeon and Physician, Discusses Bunion Surgery
.jpg)
We know that bunions are an inherited trait that can be exacerbated by activities and shoe gear. Patients can have a bunion on the inside or outside of their foot. The typical bunion is on the inside of the foot and involves the 1st metatarsal while the bunion on the outside of the foot involves the 5th metatarsal. Either pathology can often require surgical intervention in order to provide long term relief and the primary surgery is usually the bunion on the 1st metatarsal. The bunion will usually dictate the recovery and the bunion on the 5th metatarsal usually heals faster.
Bunions are typically fixed in a few ways, either a surgery at the head of the metatarsal or the base of the metatarsal. It is important to get an x-ray to examine the overall foot structure to make sure there are no other driving forces that need to be fixed. The typical foot structure we see with a bunion on both sides is a flat foot that has progressed with time. The foot often widens when a flatfoot is present to try and create more stability. The flatfoot may or may not need to be addressed.
Most bunion surgery patients will be walking the entire time after surgery and can continue with modified exercise. I utilize techniques that allow my patients to be more active and recover faster. It takes years and hundreds of patients to perfect these techniques and dealing with athletes has allowed an advantage to improve on outcomes. If you are having bunion pain please make an appointment and I will see how we can best help you. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Board Certified Surgeon & Physician
Dr Brandon Nelson, A Board-Certified Physician and Surgeon, Discuss How To Best Treat Your Heel Pain

Heel pain is the most common presenting pathology at my practice. In general, I would say 1 out of every 6 patients is for heel pain. This can be common for both adults and children. The adult usually has heel pain that is caused by plantar fasciitis and for children this is usually apophysitis or Sever’s disease.
Adult heel pain is common as one starts an exercise program or as our mileage on our feet increases. The symptoms usually begin with pain in the morning or after a walk. The feeling is often described as a bruised sensation or a burning pain. It is important to identify the underlying causes and address these. I do think an x-ray is warranted and the earlier the treatment the better.
Children usually seem to have heel pain between the ages of 10-14. The typical child has been playing sports, especially cleated sports. They usually describe a soreness that can result in limping. It is again important to take an x-ray and for underlying foot conditions.
Both plantar fasciitis and apophysitis seem to be most common in certain foot structures. These include flatfeet and tight Achilles’ tendons. I recommend stretching the calf for the tight achilles. However, the flatfoot needs to be thoroughly evaluated to prevent long term issues. I really enjoy treating both of these conditions and have great long-term protocols to eliminate this pain once and for all.
If you or your child is suffering from heel pain please call so I can help. Make an appointment online or give us a call at 425-391-8666.
Sincerely,
Board-Certified Foot & Ankle Physician & Surgeon
Dr. Brandon Nelson, Board-Certified Foot and Ankle Physician and Surgeon, Discusses Heel Pain in Kids and Adults

Pediatric heel pain or kids with heel pain are a common presentation. This heel pain is often correlated with the start of new activities or any sport season. The most common sports that heel pain occurs with children are basketball and soccer. Basketball seems to make sense as the hardwood floor can be tough and with soccer cleats seem to be an aggravating factor. It is important to have your child properly evaluated for heel pain, however the most common cause is inflammation of the growth plate. These growth plate issues are easy enough to diagnose based on clinical evaluation and radiographic findings. It is important to have x-ray heel pain because there are other causes and the treatment is tailored towards the specific pathology. Traditionally with proper implementation of a treatment plan, heel pain is usually amenable to conservative measures including clear fairly quickly.
Adult heel pain by far is most commonly caused from plantar fasciitis. Plantar fasciitis usually involves an inflammation of the plantar fascia or the supporting network of the bottom of the foot. There are many common clinical symptoms that we see each year including pain after rest or burning throbbing type sensation of the heel. Typically for adults this heel pain starts in one heel and gets worse with activities and time. Again it is important to have a thorough workup including radiographs or ultrasound examination of the heel. I believe it’s important to get in and see a foot and ankle physician fairly early in this process as this makes treatment easier. Again the majority of patients with this pathology clears up with conservative measures and returned activities.
If you suffer from heel pain or trauma suffering from heel pain I can help. Please feel free to contact the office and we will get you back on your feet pain-free. Give us a call today at 425-391-8666 or make an appointment online today.
Dr. Brandon Nelson, Board-Certified Foot and Ankle Surgeon, Discusses the Management of Morton’s Neuromas

Morton’s neuromas or interdigital neuromas are usually from a compression of the nerves in the front of the foot. Oftentimes characterized as burning or pain that’s exacerbated by walking or tight shoes. A number of different etiologies have been described to decrease blood supply progression to irritation from bursa or the intermetatarsal ligament. The majority of these neuromas occurr in the third interspace, about 70% of the time and in the second interspace about 30% of the time. It is most common to have a single neuroma however some patients have multiple neuromas. There are multiple studies on the best conservative measures.
Conservative measures range from orthotics, footwear adjustments, corticosteroid injections, alcohol injections, radiofrequency or even cryoablation. Conservative management continues to be the mainstay of neuroma therapy. Oftentimes it can take months before your neuroma feels better depending on the size and location. There are a few people that have multiple Morton’s neuroma and an MRI can be highly valuable.
Surgical management usually consists of removal of the nerve. This is generally done to the top of the foot and has a fairly short recovery as compared to other foot and ankle surgeries. Sound physicians go to the bottom of their feet just depending on experience and discomfort levels. The overall success rate with surgical management is high, if conservative measures have failed, it is the appropriate next step.
If you’re suffering from neuroma pain make an appointment today and I can help. Give us a call at 425-391-8666 or make an appointment online today.
Sincerely,
Board-Certified Foot and Ankle Physician and Surgeon
Dr. Brandon Nelson, Board-Certified Foot and Ankle Physician and Surgeon, Discusses Achilles Tendon Pain
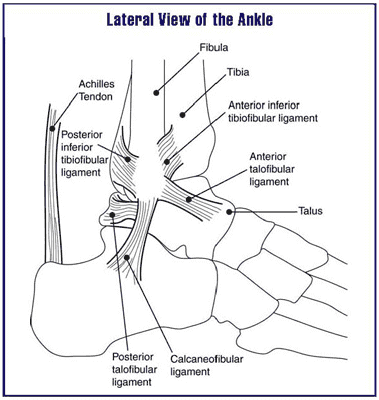
The Achilles tendon is the thickest strongest tendon in the human body. There are more pounds per square inch going across the Achilles tendon than any other tendon. It is important to realize that during an active gait cycle the Achilles tendon is under chronic mechanical load. This tendon in general can become overused and is usually attributed to an increase in activity or change in activities.
The most common cause of Achilles tendon pain is what is described as watershed region Achilles tendinitis. I encountered this in a lot of people that have begun to run or do plyometrics type activities like box jumping or jumping rope. I encouraged people not to plunge into new activities to begin to train slowly. With activities the changing and loading of the Achilles tendon can lead to Achilles tendinitis-type problems. Typically this will present as pain and swelling in the Achilles tendon. Oftentimes patients will experience increased pain that they try to push through this in addition they are at the risk of rupturing the Achilles tendon during this time.
It is extremely important that anytime a patient has Achilles tendon pain medicines evaluated by a physician. Long-term wear and tear can delay the return to normal activities. The longer patients have had these conditions there is a correlation with the longer it takes to recover. Achilles tendinopathy is one of the most common pathologies that I see if with recent developments in treatment protocols patients can return to activities sooner.
Sincerely,
Board-Certified Foot and Ankle Physician and Surgeon
Dr. Brandon Nelson, Board-Certified Foot and Ankle Physician and Surgeon, Discusses Heel pain and Plantar Fasciitis

There are quite a few causes of heel pain of heel pain and it can vary by age. We tend to break it up by pediatric meaning anybody less than 18 and adult heel pain anybody over 18. Regardless of the age and the patient heel pain can be extremely challenging and very painful. We see quite a few adults and children that are highly athletic and struggling with resolving their heel pain.
Heel pain and children is typically sourced to a disorder called calcaneal apophysitis. This is a condition where the growth plate of the heel is affected. Often times with young man this occurs between the ages of 14 and 16 and for young limited between the ages of 12 and 14. We see a high correlation with sport activities especially cleated sports. It is important to have an x-ray and follow-up with the foot and ankle physician in order to evaluate the other underlying causes.
Adults tend to have pain that occurs in the morning especially when getting out of bed or after activities. We see the majority of people have often increased their exercise routine or started a new activity. The #1 cause of heel pain and adults remains plantar fasciitis. The plantar fascia is the main supporting network of the foot and can become tired and worn out with age. Again it is important to seek help from a foot and ankle physician to determine whether or not this is the underlying cause.
Heel pain in both pediatrics and adults is highly treatable and early intervention is better. The majority of these causes can be distinguished of the first visit and felt can be implemented immediately. If you’re having heel pain please make an appointment today and I can help.
Sincerely Dr. Brandon Nelson
Board-Certified Foot and Ankle Physician and Surgeon


