issaquah podiatrist
Displaying items by tag: issaquah podiatrist
Dr. Brandon Nelson, Board-Certified Foot and Ankle Physician and Surgeon, Discusses Forefoot Capsulitis
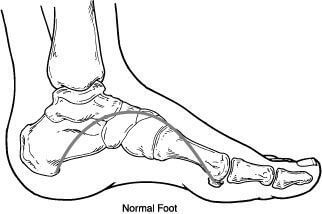
Capsulitis refers to a large group of conditions that is associated with inflammation of the joint capsule. It is important to have a little bit background of anatomy in order to understand this pathology. The joint is where 2 bones come together and these 2 bones are covered with articular cartilage and then these 2 bones are encapsulated by the joint sac that is full of fluid or hyaluronic acid. These all work in tandem to provide functional smooth gliding joint. There are many causes of capsulitis, basically it is just inflammation of the joint capsule itself.
Dr. Brandon Nelson, Board-Certified Foot and Ankle Physician and Surgeon, Discusses Heel pain and Plantar Fasciitis

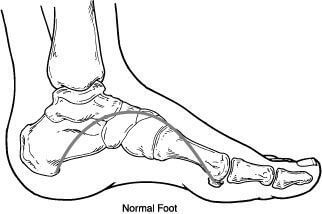
There are quite a few causes of heel pain of heel pain and it can vary by age. We tend to break it up by pediatric meaning anybody less than 18 and adult heel pain anybody over 18. Regardless of the age and the patient heel pain can be extremely challenging and very painful. We see quite a few adults and children that are highly athletic and struggling with resolving their heel pain.
Heel pain and children is typically sourced to a disorder called calcaneal apophysitis. This is a condition where the growth plate of the heel is affected. Often times with young man this occurs between the ages of 14 and 16 and for young limited between the ages of 12 and 14. We see a high correlation with sport activities especially cleated sports. It is important to have an x-ray and follow-up with the foot and ankle physician in order to evaluate the other underlying causes.
Adults tend to have pain that occurs in the morning especially when getting out of bed or after activities. We see the majority of people have often increased their exercise routine or started a new activity. The #1 cause of heel pain and adults remains plantar fasciitis. The plantar fascia is the main supporting network of the foot and can become tired and worn out with age. Again it is important to seek help from a foot and ankle physician to determine whether or not this is the underlying cause.
Heel pain in both pediatrics and adults is highly treatable and early intervention is better. The majority of these causes can be distinguished of the first visit and felt can be implemented immediately. If you’re having heel pain please make an appointment today and I can help.
Sincerely Dr. Brandon Nelson
Board-Certified Foot and Ankle Physician and SurgeonDr Timothy Young Talks About Tight Calves and Foot Problems, Part 2
Tight calves and Achilles are a major factor in many foot problems. That is why we use a night splint and calf stretching is helpful for many problems. Problems in the front of the foot like 2nd toe capsulitis metatarsalgia often respond well to calf stretching. We have discussed how during gait, early heel rising and transfer of weight to the front of the foot can increase the load and weight transfer to the forefoot (and midfoot). This early transfer of weight and mechanical load can be destructive.
With our example of capsulitis of the 2nd toe, we now have an extra load going through the 2nd metatarsal and toe joint. Eventually the extra load can strain the 2nd metatarsal and capsule. This can lead to capsulitis or even a stress fracture of the metatarsal. So, to help with this, we have our patients stretch their calf and use a night splint. We avoid shoes that further put more pressure on the front of the foot (like high heeled shoes). We even recommend shoes with zero heel drop, like Altra shoes. This is just one example of how equinus can factor into a foot problem, there are so many more examples where this happens. So, this is just the “tip of the iceberg” as a major factor in many foot problems and pathology. Keeping your calf stretched out is one of the single best exercises you can do to keep your feet healthy!
If you are experiencing foot or ankle pain, give us a call today at 425-391-8666 or make an appointment online.
Dr Brandon Nelson, A Board Certified Surgeon, Discusses The Best Questions To Ask Your Surgeon Before Having Bunion Surgery

I try to let my patients know that I understand how scary or nervous it can feel to think about surgery. I think as surgeons sometimes we can forget that for us this is routine, however for the patient it can seem overwhelming. Bunion surgery itself is relatively straight forward and can provide great results. I have thought it could be helpful to have a few questions to ask your surgeon.
I think one of the most important questions to ask your surgeon is, “How many bunion surgeries you have done and how often you do them?”. I think most likely you are seeing a Podiatrist and we perform the most bunion surgeries out of any other specialty. I can tell you in residency alone I probably did over 500 and now into private practice for over 10 years I am sure the number is over 1000.
Another important question is, “What are some of the most common complications that occur?”. Every surgery has complications this is part of practicing medicine. The most important aspect of this is how they handle it and how quickly a surgeon responds to these. One of the most common is probably infection and this is rare, the literature state about 3% of all patients will experience this.
Additional question could include, “Why did you select this procedure?” There are numerous different bunion procedures and why we select a particular one is important. This is because they all have different correction abilities and time frames for healing. The majority of bunion procedures can be categorized as head or base procedures. Lastly, “What is my recovery time?”, be specific are you talking about back to exercising or just into a normal shoe.
I hope this was helpful, please feel free to schedule an appointment with me if you would like a consultation of second opinion. Give our office a call at 425-391-8666.
Dr. Brandon Nelson, A Board Certified Surgeon, Discusses Neuroma Surgery
Neuromas are a common presenting pathology in my office. I see quite a few in the typical week. The majority of patients with neuromas are female between the ages of 40-60. The patient will usually describe burning or tingling in the foot that is worse with shoes. Most of the time on exam one can feel the nerve moving, this is called a “Molder’s click”. I will usually get an x-ray and then help the patient with a long-term plan.
There are a few conservative modalities that work fairly well for a neuroma and I usually recommend trying these before proceeding to surgery. However, often times patients have tried these and are seeing me as a second opinion.
Surgery is relatively straight forward for a neuroma. The majority of us use a incision on the top of the foot that is about 3 inches long and provides great exposure to the nerve. The nerve is removed, and the entire procedure takes about 15 minutes. I let my patients walk after surgery and most are able to tolerate the discomfort from surgery with just an oral anti-inflammatory.
If you have burning or tingling in your foot or have been diagnosed with a neuroma I can help. Make an appointment today and we can review your options and get you back on your feet pain free.
Give us a call at 425-391-8666.
Mid Foot Bone Spurs and Surgery Part Two
Mid foot bone spurs and surgery part two.
Surgery to treat a bony prominence in this area usually is very straightforward. It typically involves an incision directly adjacent to the prominence or bone spur. We surgically go down to the tissue layers and then expose the bony prominence. Then most commonly a power burr is used to smooth down the excessive bone in the area or sometimes a special surgical saw. The wound is cleaned up and flushed to remove any small bone fragments.
The remaining cut bony surface usually has an excellent blood supply and can cause swelling problems or even a small collection of blood like a hematoma. Therefore several different techniques can help deal with this. One is to use a small drain which allows for a path for the blood to escape the area, this is especially useful for the first several days postop. Another strategy is to use bone wax to seal the bone.
Some Surgeons use topical fibrin to help clot exposed bleeding vessels that are small and embedded in the bone. After the bone remodeling procedure is done, the soft tissue layers are closed and the procedure is then complete. Usually it’s a relatively quick recovery. Remember that we are talking about a bony prominence without significant underlying midfoot arthritis. The midfoot arthritis and surgical fusion of the involved joint can be a longer recovery.
If you have questions about spurs or bumps on the top of your feet forefoot surgery in general, and would like a consultation please let us know. Give us a call at 425-391-8666 or make an appointment online.
Dr. Brandon Nelson, A Board Certified Physician, Discusses Achilles Tendon Pain
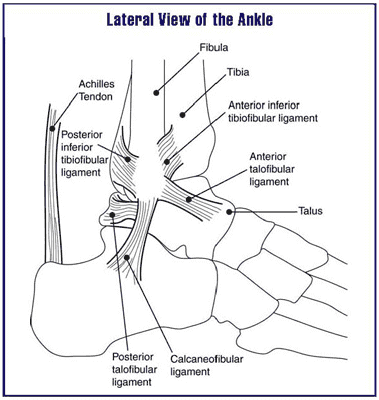
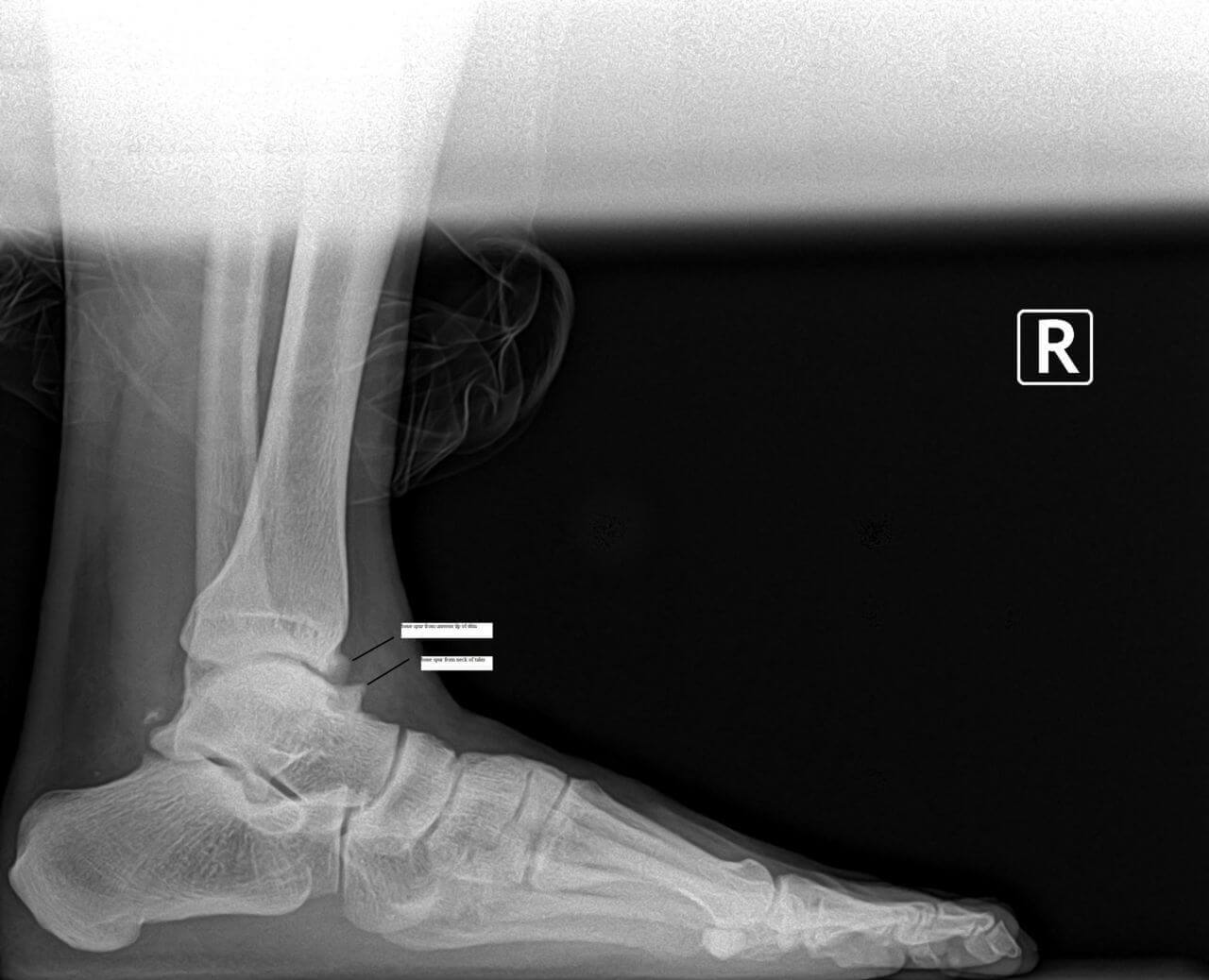
The Achilles tendon is the thickest and strongest tendon in the human body. It has more pounds per square inch applied to it than any other tendon. We consider it the work horse of the lower extremity. It is constantly in use and provides forward motion in the gait cycle. These reasons make it one of the most commonly injured or strained tendons.
Achilles tendonitis usually presents with pain and selling around the back of the ankle. Patients have usually increased activities or changed activities or even started to walk more. There is often pain when getting out of bed, that gets better as the day goes on, but returns with rest. Sometimes patients will describe weakness or a catching sensation.
Diagnosing Achilles Tendon injuries is relatively straight forward. A typical mechanical and musculoskeletal exam of the foot and ankle are performed. An ultrasound or x-ray can be helpful as well. More advanced cases can require an MRI to rule our tearing or degeneration.
Treatment is provided on a case-by-case basis. It is important to identify the cause and help eliminate or reduce this activity. Stretching is vital and reducing the mechanical burden. I always encourage people with Achilles issues to see a foot and ankle physician before implementing treatment as these measures are not always appropriate. If you are suffering from Achilles tendonitis, give us a call at 425-391-8666 or make an appointment online so we can get you back on the road to recovery.
Dr. Brandon Nelson, a Board Certified Physician, Discusses Achilles Tendonitis
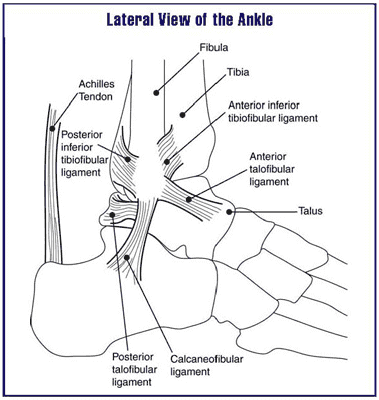
The Achilles tendon is the work horse of the lower extremity. It provides forward propulsion and is the thickest, strongest tendon in the human body. It basically never has a chance to rest if you are walking. The tendon itself is made of three different muscles and contracts to provide power. That is why it is one of the most common tendons to experience tendonitis in.
It is probably the most common type of tendonitis we see in the office. I would also say it is one of the most challenging to treat. The challenge is it's constantly in use and the number one cause of Achilles tendonitis is overuse. We see a fair amount as the summer starts and people get outside. The other big culprit is a new exercise program. Most of these patients are usually men and around the age of 40.
I encourage patients to get in early and treat this aggressively. The Achilles tendon is notorious for taking a long time to return to a normal state and recover from tendonitis. The earlier and more aggressive the treatment the better the long-term outcomes. Focusing on eliminating the abnormal pull of the Achilles and stretching provide relief. There are numerous opportunities to administer more advanced treatment options that utilize the body's own ability to heal. These techniques seem to have the best long term outcomes. If you are suffering from Achilles’ tendon pain we can help.
Give us a call at 425-391-8666 or make an appointment online today.
Dr. Brandon Nelson, A Board Certified Physician, Discusses Metatarsalgia And Foot Filler For Fat Pad Atrophy
Metatarsalgia refers to pain and inflammation under the metatarsal heads in the foot. Patients often experience burning or tingling or even bruised type sensations in the ball of the foot with walking and exercise. This is often caused by the lose of fat pad or cushioning in the foot. This can occur as a normal aging process or as a genetic predisposition.
One of the best options available to treat fat pad atrophy or loss of fat pad or metatarsalgia are foot fillers. These foot fillers can be used to replace natural cushioning in the foot. There are many different types of foot fillers. I prefer to use adipose tissue as it is a naturally occurring product and provides no immune response. Adipose transplant can be highly effective long term and can be preformed in the office with local anesthetic. Most people find significant relief for long periods and have very little down time.
If you have metatarsalgia or loss of fat pad, contact my office today and request a consultation.
Give us a call at 425-391-8666 or make an appointment online today.
Bunion Surgery and Bunion Correctors, Dr. Brandon Nelson, a Board Certified Bunion Surgeon, Discusses Both
.jpg)
Bunions are a common pathology that presents to my practice. The majority of bunions are seen on women between the ages of 30-50. Most have noticed the bunion at an early age and slowly have noticed them grow. A lot of patients feel their shoe selection has contributed to the growth or their activities like running. We know that bunions are an inherited foot structure that gets worse with time and usage.
Bunion correctors are common on the internet and I have seen them all. What we know about bunion correctors are they can help relieve some pain that is related to soft tissue contractures. The bunion itself is a bony malalignment of the foot and the bunion corrector cannot move bone back into position. The bunion corrector can help stretch some of the soft tissues as the bunion gets larger. However, it should be noted no bunion split or corrector will fix you bunion or change the shape of your bunion.
Bunion surgery is the only way to realign the bones that cause a bunion. I recommend bunion surgery for anybody that is having pain or difficulty fitting shoes. I consult and hundreds of bunions a year and can tell you that they are not all the same. It is very important to have a complete workup including physical exam and x-ray of the bunion. Proper procedure selection is key to fixing the bunion correctly.
If you are experiencing bunion pain and would like a consultation please call us at 425-391-8666 or make an appointment online and I will review all your options from conservative to surgical at your appointment.



