bfdadmin
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses the Best Options for Bunion Surgery
.jpg)
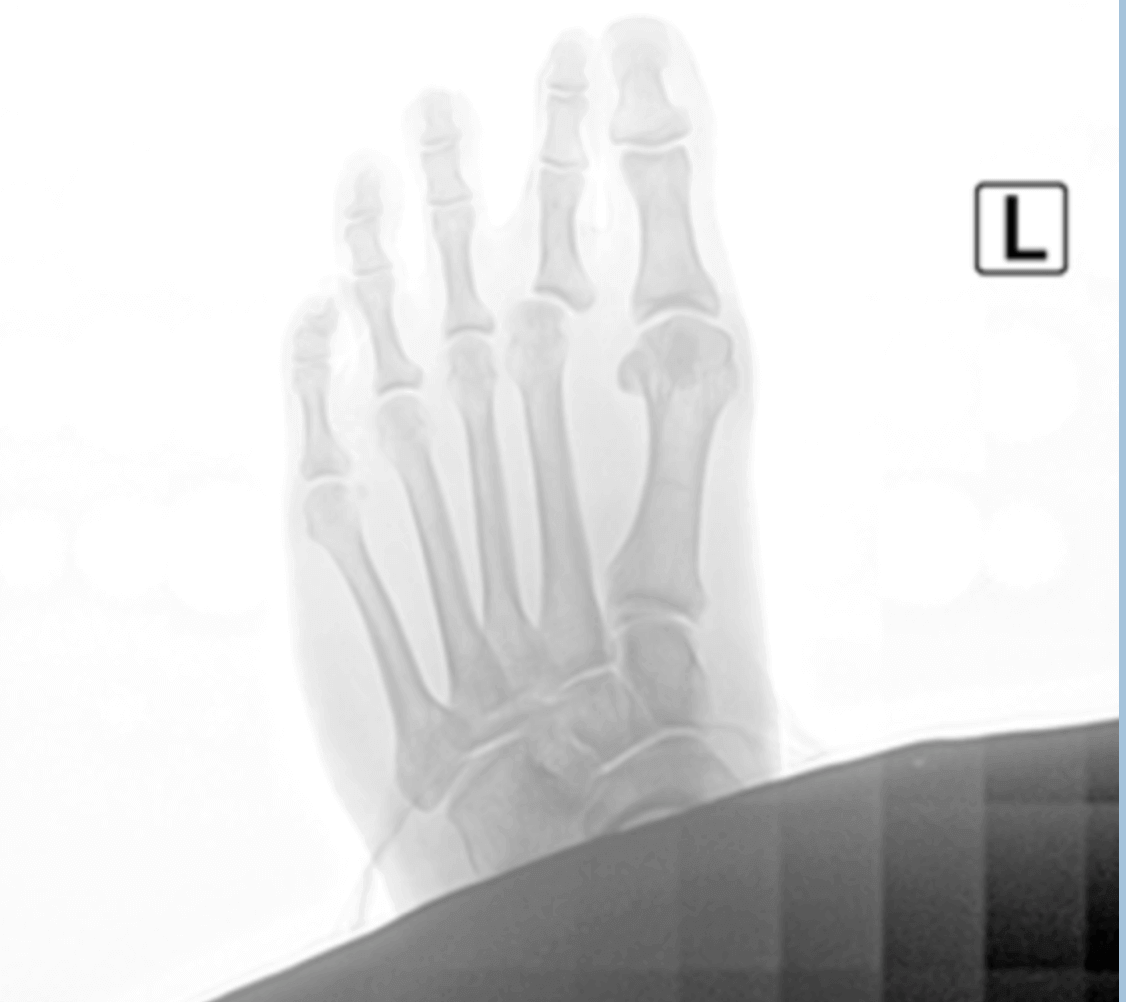
Bunions are present in many different sizes and shapes. I see bunions on the inside of the foot, the outside of the foot and both. It is important to remember that some small ones can be painful, and some large ones can be pain free. It often seems to be dependent upon activity levels and shoe gear. If they hurt or limit your lifestyle then maybe it is time to fix them.
Fixing your bunion
Bunion surgery has two main procedures that are done. One is what is called a head procedure. This is basically cutting the bone and realigning it through transposition of the bone. Usually fixated with one or two screws. The other involves fusion of a joint, specifically the joint that is involved with the creation of the bunion. This procedure is called a Lapidus bunionectomy.
Bunion recovery
Recovery really depends on the procedure that is performed. Head procedures recover faster and usually involve no periods of non-weight bearing. The fusions often involve a period of crutches or knee scooters. This can be as short as 3 weeks or as long as 10 weeks. The weight bearing status can be dictated by other procedures that are done as well.
Which bunion surgery is right for me?
This is a hard question to answer. I believe this is where your consultation with your surgeon is extremely important. Other factors like lifestyle, recovery support, expectations and experience can play a major role. I think it is important to get an entire overview of the process and have a discussion with your surgeon.
If you would like a consultation for your bunion I can help. Call to make an appointment with me at 425-391-8666 or make an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Plantar Fasciitis

Plantar fasciitis affects millions of people worldwide. It is often a debilitating condition that limits people’s activities. It is characterized by pain in one’s heel, pain when we get out of bed or can even be a bruised sensation to the bottom of the foot. Today I will discuss some of the causes, symptoms, diagnosis, and treatment. The plantar fascia itself is a thick ligament like tissue that runs on the bottom of the foot to provide support.
Causes:
The number one cause is overuse. This can be exercise or standing all day or a change in the amount of either of these. Other causes can be shoe gear, weight or even the foot structure one is born with.
Symptoms:
The most common symptom is sharp heel pain, especially when you first get up from a seated position. This usually improves as we walk but returns at the end of the day. Some people experience stiffness or even burning.
Diagnosis:
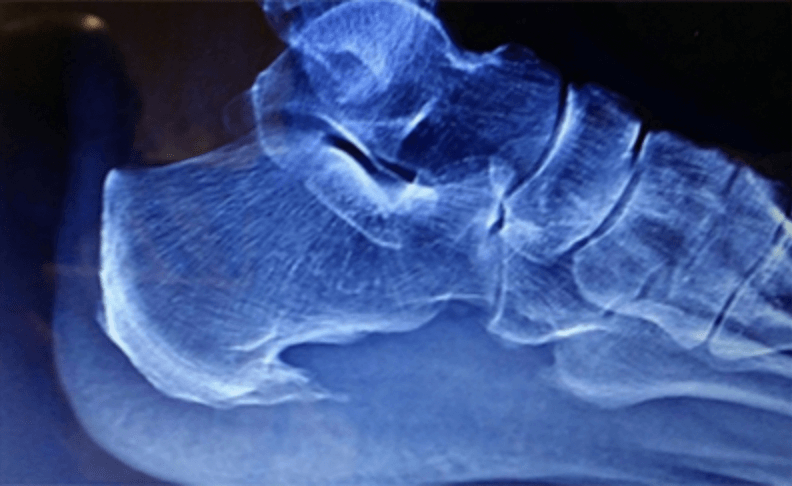
A good clinical examination can help identify plantar fasciitis for most people. The is usually pain with palpation of the heel, specifically at the heel bone where the fascia attaches. An x-ray can be useful to detect bone spurs.
Treatment:
The mainstay of treatment is to work on stretching of the foot and Achilles. Additionally, increasing support for the feet can be helpful. Often by the time I see patients an injection is needed to calm down the inflammation and help with recovery.
If you would like a consultation on your heel pain, I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
Dr Brandon Nelson
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Plantar Fasciitis

Plantar fasciitis or heel pain is the most common cause to seek help from a foot and ankle physician. There are many causes of heel pain but by far the most common is plantar fasciitis. So, let’s discuss first what the plantar fascia is, second why it occur and lastly how to fix it.
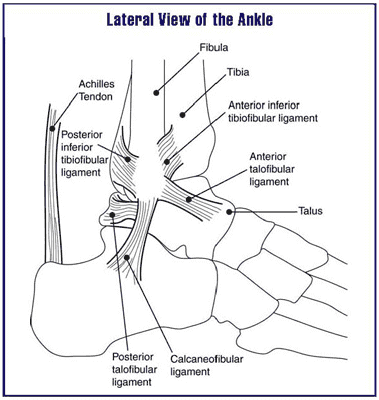
What is your plantar fascia? The plantar fascia is located on the bottom of your foot. It runs the entire length of your foot from your heel to your toes. It starts with an attachment at the calcaneus, your heel bone, and runs to your metatarsal head, where your toes start. It is a thick dense fascial type of tissue. Its main function is to support your arch. It also helps flex your toes and provides stability to your foot with ambulation.
Why does plantar fasciitis happen? There are many schools of thought on this one but let’s talk about a few of the most common. The first and probably most accepted theory is overuse. The fascia never gets a chance to rest, it is the workhorse of the foot. Every step you take it is activated and over time this can fatigue the structure. Secondly foot genetics can play a role in it as well. People with a flatfoot tend to need more arch support and this can put pressure on the plantar fascia. Lastly there is a thought that tight calf muscles can pull on the fascia making it irritated. I think all of these can have merit in certain circumstances and I often see multiple etiologies.
Lastly, how do we treat plantar fasciitis? This is a more complex question. I think this one is very hard to answer as every case can be different. I think a careful history and physical is essential for proper treatment. I also find length of time and activity level to be important. But a couple general things can help like calf stretching and activity medication can be essential.
If you would like a consultation on your heel pain, I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online today.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Heel Pain and When to See A Foot & Ankle Specialist

Are you currently suffering with heel pain? I can remember those days not long ago for me. I would wake up in the morning and that first step pain was terrible. It would take a couple minutes and it would finally loosen up only to return every time I sat down. Does this sound familiar? If so, you probably have plantar fasciitis. The big question is when to see a foot and ankle specialist, the answer is now.
The sooner you get in to seek treatment the faster your recovery will be. With procrastination the inflammation gets worse, and you will take longer to recover. I tell all my patients the sooner we initiate treatment the faster we can get you back to enjoying the things you like.
Treatment of plantar fasciitis usually starts with a review of your activities. What are you currently doing for exercise and how often? Have there been any recent changes? I like to get an x-ray to check for bone spurs and arthritis. A good overall examination of the foot structure and lower leg can be helpful along with any treatments that have been tried. If the diagnosis is still plantar fasciitis then the average patient I see will be about 50% better in less than a week with the first line of therapy.
If you have heel pain, you know how uncomfortable it can be. If you would like a consultation on your heel pain, I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
Dr Brandon Nelson
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Discuss What To Expect After The Lapiplasty Bunion Correction

There is a lot of talk about the lapiplasty procedure for bunion correction. I think it is important to spend a minute and look at the history and what exactly the procedure is. Then we can discuss the expectations after surgery.
The lapiplasty is based on the lapidus bunionectomy. This is a procedure that was first described by Dr Paul Lapidus. This surgical correction for bunions has been around for about 100 years. It has been shown to be the most effective method to correct a bunion. The trouble with it is it can be technically difficult to perform and has a long recovery. Most of us foot and ankle surgeons trained utilizing this procedure especially if you trained on the West Coast. Seattle, where I trained is the epicenter for the lapidus procedure.
What is the lapidus procedure? The procedure itself involves correcting a bunion at the apex of the deformity. Most of us believe this is at the tarsometatarsal joint. This is where the correction occurs with the lapidus and lapiplasty. The procedure involves, releasing the 1st metatarsal joint and sesamoid, correcting the metatarsal and then fusing the tarsometatarsal joint. This fusion was the limiting step to recovery and this is where the lapiplasty surgical set has made steps to decrease healing times. Their system utilizes a plate that allows early weight bearing.
Recovery for most patients undergoing a lapiplasty can be summarized as follows;
-First week couch potato, relax put your foot up
-Week two get your dressing changed
-Week three start weight bearing in the boot
-Week 6 begin to transition out of boot into normal shoe
-Month 3 back to full activities
If you have a bunion and would like to discuss the Lapiplasty make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
Board Certified Foot & Ankle Surgeon
Dr. Timothy Young, a Board-certified Foot Surgeon discusses bone spurs in the foot: Osteophytes
Dr. Timothy Young, a Board-certified Foot Surgeon discusses bone spurs in the foot: Osteophytes
Defining Osteophytes: Osteophytes, a subset of bone spurs, are characterized by the outgrowth of new bone on the margins of a synovial joint. They often develop in response to joint degeneration and are associated with conditions like osteoarthritis.
Locations of Foot Osteophytes:
1. Joints: Osteophytes often form on the margins of joints of the foot, impacting movement and causing pain.
2. Edges of Bones: They may also develop along the edges of bones, affecting the alignment of joints.
Causes and Risk Factors:
1. Joint Degeneration: Osteoarthritis, a common cause of bone spurs, leads to the breakdown of cartilage and prompts the body to form osteophytes.
2. Repetitive Stress: Continuous mechanical stress on specific areas of the foot, often due to poor biomechanics or ill-fitting footwear, can contribute to the development of bone spurs. This often involves the force of gravity on weight-bearing joints. A good example would be the ankle joint.
Symptoms and Diagnosis:
1. Pain: Persistent pain in the affected area, especially during movement or weight-bearing activities.
2. Reduced Range of Motion: Difficulty moving the affected joint due to the presence of bone spurs.
3. Visible Bumps: In some cases, visible or palpable bumps may be present, indicating the presence of bone spurs. A good example this would be a bump on the top the midfoot that is due to large osteophytes in this location.
4. X-rays and ultrasound: x-rays and ultrasound can show the osteophytes. It is usually not necessary to do an MRI or CT scan.
Treatment Options:
1. Conservative Measures:
- Rest, ice, compression, and elevation (R.I.C.E.).
- Orthotic inserts and supportive footwear.
2. Physical Therapy:
- Stretching and strengthening exercises.
- Therapeutic modalities to alleviate pain and inflammation.
3. Medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain management.
4. Injections: injections can deliver medication such as Supartz which is a synthetic joint lubricant. This was originally FDA approved for the knee but is now used throughout the body. For the foot and ankle, it is most commonly used in the ankle joint and the great toe joint. Cortisone is not used as often, since repetitive use can weaken the existing Cartledge and adjacent joint capsule.
- In severe cases, surgical removal of the bone spur may be considered, or in some cases the joint can be stabilized by fusing it or placing an implant in the joint.
Conclusion:
Bone spurs and osteophytes in the foot can present challenges, but with proper understanding and timely intervention, individuals can manage their symptoms effectively. If you suspect the presence of bone spurs in your foot, please contact our clinic and we can review your options.
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses How To Make Sure You Have a Successful Bunion Surgery
.jpg)
Bunion surgery is one of the most common surgeries performed in the United States. It is something like 250,000 operations annually, that is a lot of bunions! Well, how can you maximize your results, get back to activities early and heal faster? I will give you some insight on these questions.
Maximizing bunion results, when I think about what this question means I think it would pertain to how you get the best outcomes. This means to me how you make the foot more functional and get a good cosmetic result. This would be best done through appropriate procedure selection. There are a lot of different bunion operations that are used to fix different sizes of bunions and different foot structures. To me the most important thing here is to select a bunion surgeon that does a lot of bunions.
How do you get back to activities earlier? The main point here is to follow your surgeon's protocol. Do not listen to your neighbor or friend, they might have had a different operation than you. Your surgeon really knows best in this case. Most of us have taken years to perfect our post-op protocol and do not deviate from following them to the letter. But if you have questions or concerns ask to let us know.
Healing faster can mean a lot of things, the skin, the bone, when one can walk. The skin is the first thing to heal. I always recommend collagen and zinc supplements. These seem to speed things along and once the incision is closed there are some great products to minimize scar appearance. Next is the bone, a good bone healing supplement is essential and if available a bone stimulator can shave weeks off healing. Weight bearing is a different story, often this depends on other procedures that were done. I try to get all my patients moving and bearing weight within a couple days if appropriate. The minimum is to start a range of motion exercises.
If you would like a consultation on your bunion, I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Tips To Get Ready For Bunion Surgery
Bunion surgery is the most common surgical procedure I perform at my ambulatory surgery center. I have a few tips I would like to share that can make things much easier.
Get ready a week before surgery. Start thinking about where you will set up. I always recommend being a couch potato for about a week. This home base spot should be conveniently located. This spot should be downstairs and near a restroom. Make sure you have access to anything that might pass the time, a computer, tv, etc.
Meals are another thing to think about. I like to advise my patients to make a weeks’ worth of food. You can freeze them or refrigerate them but not having to cook can be a game changer. This can really help you focus on your recovery, and nobody wants to cook with a sore foot.
Supplements are another thing to consider. I think talking to your surgeon about this one is important. Calcium or some sort of bone healing supplement if you are having bone work done. Collagen and zinc can help wound healing. Once the wound closes, start topical scar care.
The bathroom situation can need some thought as well. How will you shower or use the toilet? I always if you are going to be non-weight bearing to have a trial run of both. It can be difficult executing these tasks with one foot. Options for these include a shower chair or stool and for the toilet they make elevated seats that are helpful.
Medications are the last thing I will touch on. Get these before the day of your procedure. Think about making a log or schedule so you can track what and when you take them. Make sure you understand what each is and that you have no interactions with other medications you are taking.
If you would like a consultation on your bunion, I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses The Benefits of Having The Lapiplasty Bunionectomy

I remember performing my first bunion surgery over 15 years ago and was so excited to help my patient. I also remember learning all the different types of bunion surgeries and how each one was slightly different. It made me ponder why there were so many different types of bunion surgeries for one pathology. It was about this time I was introduced to the Lapidus bunionectomy by an attending physician. He discussed how this was his favorite procedure, how it provided great outcomes but was difficult to execute.
Well fast forward 15 years and now the Lapidus is one of the most common bunion surgeries in the United States. Things have really changed with the Lapiplasty system. A group of doctors worked with a medical device company to develop a series of gigs and clamps to make the Lapidus reproducible and easier to perform. This has really revolutionized bunion surgery and I anticipate Lapidus will eventually be the most common surgery worldwide.
I feel lucky having trained in the Northwest as I am very familiar with the Lapidus procedure and even before the Lapiplasty system it was one of my go to bunion corrections.
If you have a bunion, you know how uncomfortable they can be. If you would like a consultation on your bunion I can help. Call to make an appointment with me at 425-391-8666 or schedule an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Timothy Young, a Board-certified Foot Surgeon Discusses Tenex Procedure for Achilles Tendonitis: A Revolutionary Approach to Healing
Dr Timothy Young, a Board-certified Foot Surgeon Discusses Tenex Procedure for Achilles Tendonitis: A Revolutionary Approach to Healing
Introduction:
Achilles tendonitis is a common condition that occurs when the Achilles tendon, the large tendon connecting the calf muscles to the heel bone, becomes inflamed and causes pain and discomfort. Achilles tendinosis is a more accurate term when there is thickening of the tendon itself with degenerative changes within the tendon. Traditional treatment methods often involve rest, physical therapy, and anti-inflammatory medications. However, for those seeking a more advanced and minimally invasive solution, the Tenex procedure has emerged as a groundbreaking option. Furthermore the Achilles tendon problems can involve the insertion of the tendon lower at the heel, or further up above the heel. In either case these can be chronic painful conditions.
What is the Tenex Procedure?
The Tenex procedure, also known as percutaneous tenotomy or TX1 MicroTip technology, is a minimally invasive treatment designed to target and remove damaged tissue in the Achilles tendon. This is especially effective for Achilles tendinosis. This cutting-edge approach can effectively alleviate pain and promote the natural healing process without the need for open surgery.
How Does the Tenex Procedure Work?
The Tenex procedure utilizes ultrasonic energy to precisely target and break down diseased or damaged tissue within the Achilles tendon. Overall the non-damaged portions of the Achilles tendon left intact which speeds the overall healing. The process involves the following key steps:
1. Diagnosis: Before recommending the Tenex procedure, a thorough evaluation of the patient's condition is conducted, typically including imaging studies such as ultrasound or MRI to pinpoint the location and extent of the tendon damage.
2. Local Anesthesia or IV sedation combination: The patient is given local anesthesia to numb the targeted area, ensuring a pain-free experience during the procedure.
3. Ultrasonic Energy Application: A small incision is made to access the damaged area. A specialized ultrasonic tool is then inserted through the incision, delivering precise ultrasonic energy to break down and remove the damaged tissue without affecting healthy surrounding tissue.
4. Aspiration: Simultaneously, a suction mechanism removes the broken-down tissue, promoting the body's natural healing response.
5. Minimal Scarring: Due to the minimally invasive nature of the procedure, scarring is typically minimal, and the recovery period is shorter compared to traditional open surgery.
Benefits of the Tenex Procedure:
1. Minimally Invasive: The Tenex procedure is performed through small incisions, reducing the risk of infection, minimizing scarring, and allowing for a quicker recovery.
2. Targeted Treatment: The ultrasonic energy precisely targets and removes damaged tissue, preserving healthy tendon fibers and promoting more effective healing.
3. Outpatient Procedure: The Tenex procedure can be performed on an outpatient basis, allowing patients to return home the same day.
4. Quick Recovery: Patients often experience a faster recovery compared to traditional surgical methods, enabling them to resume normal activities sooner.
5. High Success Rate: Clinical studies have shown positive outcomes and high patient satisfaction rates with the Tenex procedure, making it a great option for those suffering from recalcitrant Achilles tendonitis.
Conclusion:
The Tenex procedure represents a significant advancement in the treatment of Achilles tendonitis, offering a minimally invasive and targeted approach to alleviate pain and promote healing. As with any medical procedure, it is essential to consult with a qualified healthcare professional to determine the most suitable treatment plan based on individual needs and circumstances. With the Tenex procedure, individuals may find a path to recovery that aligns with their desire for effective, efficient, and minimally disruptive treatment. If you have Achilles tendon symptoms please consider a consultation at our clinic. Achilles tendon evaluation and treatment is a specialty at our clinic.
Give us a call at 425-391-8666 or make an appointment online today.



