bfdadmin
Dr Brandon Nelson, A Double Board Certified Physician and Surgeon, Discusses Bunion Surgery Questions
Every week a few patients come in wondering about having their bunion fixed. I really enjoy these discussions and helping patients decide what is best for them. There are quite a few common questions I get so I decided to answer them in this blog
1. How much time will I need to be off my feet?
This question really depends on what procedure is utilized to correct your bunion as well as any additional procedures performed. It can be as little as a few days or up to 6 weeks. I like to get my patients walking as quickly as possible.
2. When can I start to exercise?
Again this is a tough one to answer. But, I am an avid exerciser and know how important it is to maintain our current levels and not lose too much ground with time off. I like to help my patients develop a post-operative plan to continue working out and modify activities.
3. When will I be back in a normal shoe?
This again depends on other procedures performed and how much work was needed to correct your bunion. I see some patients back in a normal shoe at 4 weeks and some as long as 10 weeks. The best thing you can do as a patient is follow your post-operative instructions.
4. Will my bunion recur?
I always recommend seeing a physician that does quite a few bunion surgeries as this will give you better outcomes. Procedure selection is the most important component to decrease recurrence rates. With proper selection recurrence rates are about 2-3%.
If you have a bunion and would like a consultation please call 425-391-8666 and make an appointment online.
Sincerely,
Foot & Ankle Surgeon
Issaquah’s Top Podiatrist
Dr. Timothy Young a board-certified foot surgeon discusses Chillblains: causes, symptoms, and treatment.

Introduction: As winter settles in, along with its frosty bite, many of us bundle up in layers of clothing to protect ourselves from the cold. Despite our efforts, some may still find themselves facing an uncomfortable and sometimes painful condition known as chillblains. Chillblains, also spelled chilblains, are a common affliction during colder months, yet they remain relatively misunderstood. Chilblains is the common term used for this and Pernio is the medical term for chilblains. Very similar conditions include Raynaulds phenomenon and acral cyanosis. In this blog post, we discussed the details of chillblains, exploring their causes, symptoms, and effective treatments.
What are Chillblains? Chillblains, medically termed pernio, are a localized reaction of the skin to cold temperatures. They occur when the skin is exposed to cold but not freezing temperatures and then undergoes rapid warming, causing blood vessels to expand and leak. This leakage leads to inflammation and injury to the surrounding tissues.
Causes of Chillblains: Chillblains typically develop in response to repeated exposure to cold, damp conditions. Individuals living in cold climates or those who spend prolonged periods outdoors during winter are at higher risk. Certain factors may predispose individuals to chillblains, including poor circulation, hormonal changes, and medical conditions such as Raynaud's disease.
Discussion: Vasospasm of the smaller blood vessels in the digits are common in this case pulses in the feet may be intact but despite this the blood flow to the digits is essentially cut off. With a lack of oxygen there can be tissue damage and resultant inflammation even after the blood flow is reestablished. It also can be common for the individual’s foot to be moist from perspiration such that a “damp chill” on the feet occurs. This is why one of the strategies is to keep the feet dry and wool socks do a great job with this. In addition in the toes if there is a place where the toes often rub together that seems to be a common location to get purple/cyanotic nodular enlargement and irritation from the contact between the toes. Patient will come into the clinic with these purple painful nodules on their toes and states that they been to other clinics and owns quite certain what it is. They commonly think that they started out as a blisters.
Symptoms of Chillblains: The symptoms of chillblains can vary in severity but commonly include:
- Redness or purplish discoloration of the skin
- Swelling and tenderness with nodular enlargement
- Itching or burning sensation
- Blistering or ulceration in severe cases, often these are purple or cyanotic.
- Pain or discomfort, particularly upon warming the affected area
Chillblains most commonly affect the extremities, such as the toes, fingers, ears, and nose, but can also appear on other parts of the body exposed to the cold.
Treatment and Management: While chillblains can be uncomfortable, they typically resolve on their own within a few weeks once the affected individual is no longer exposed to cold temperatures. It’s not uncommon for these to last often on through the winter and then totally resolved each summer. But as the years go by sometimes the become progressively more of a challenge or problem. However, several measures can help alleviate symptoms and promote healing:
- Keep the affected area warm but avoid sudden temperature changes.
- Gently massage the area to improve circulation.
- Apply soothing lotions or creams to relieve itching and discomfort.
- Avoid scratching or rubbing the affected skin to prevent further irritation.
- Protect the skin from further exposure to cold and moisture by wearing appropriate clothing and using gloves, socks, or earmuffs.
In more severe cases or if complications arise, medical intervention may be necessary. This may include prescription medications to reduce inflammation, promote healing, or manage underlying conditions contributing to poor circulation.
Prevention: Prevention is key to avoiding the discomfort of chillblains. Some tips to prevent chillblains include:
- Dress warmly in layers, paying particular attention to extremities.
- Keep indoor environments warm and dry, especially during colder months.
- Limit exposure to cold and damp conditions, and take breaks to warm up if spending extended periods outdoors.
- Wear moisture-wicking socks and breathable footwear to prevent moisture buildup.
- Maintain good circulation through regular exercise and avoiding tight-fitting clothing or accessories that may restrict blood flow.
Conclusion: Chillblains are a common but often misunderstood condition that can cause discomfort during colder months. By understanding the causes, symptoms, and effective treatment options, individuals can better manage and prevent chillblains, ensuring a more comfortable and enjoyable winter season. If symptoms persist or worsen, it's essential to seek medical advice for proper evaluation and treatment. Remember, staying warm and dry is key to keeping chillblains at bay.
If you have any questions or would like a consultation please call 425-391-8666 and make an appointment online.
Foot & Ankle Surgeon
Issaquah’s Top Podiatrist
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Why He Has Been Fixing Heel Pain For Over 15 Years
Heel pain is usually caused from inflammation of your plantar fascia. However, this is not the only cause of heel pain. Other causes can include arthritis, nerve irritation, bursal sacs and even mechanical foot collapse. I always recommend physician intervention as things will subside much faster.
Plantar fasciitis is characterized by pain in the morning or after rest. Most patients have increased activities or spend a lot of time on their feet. The pain can feel like a bruise or throbbing that can extend from the heel to the arch. This can go on for months before patients seek treatment or even years. But remember the sooner you see a foot and ankle physician the faster the recovery and return to normal activities.
The mainstays of heel pain treatment are stretching and icing. It is important to get a correct diagnosis before starting any treatment as somethings can exacerbate heel pain and make symptoms worse. An x-ray and careful physical examination are essential to helping discover the underlying causes of heel pain. Assuming all heel pain is plantar fasciitis is a mistake. I have been treating heel pain for over 15 years and have a protocol so successful that most patients are 70% better in less than a week.
Do not let heel pain control your life. How long have you been suffering? Call today and let me help you get better. If you would like a consultation for your heel pain I can help. Call to make an appointment with me at 425-391-8666 or make an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses the Lapiplasty Bunion Correction

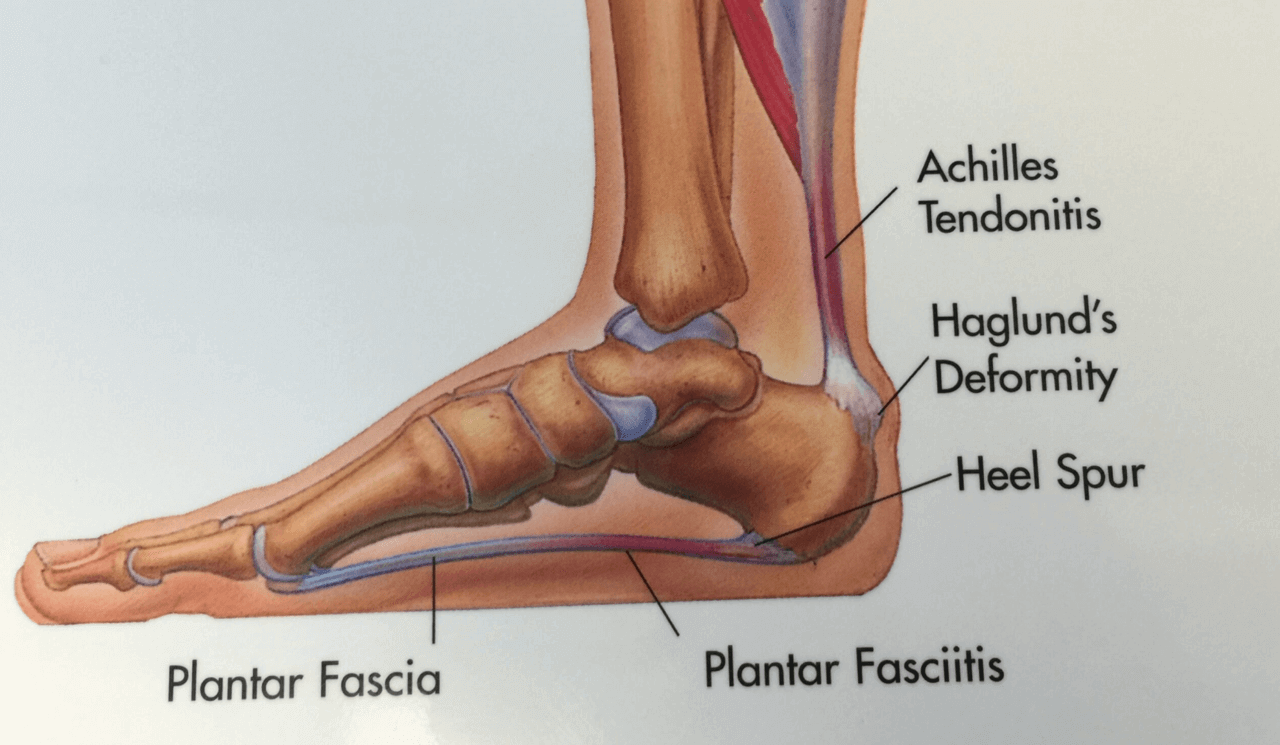
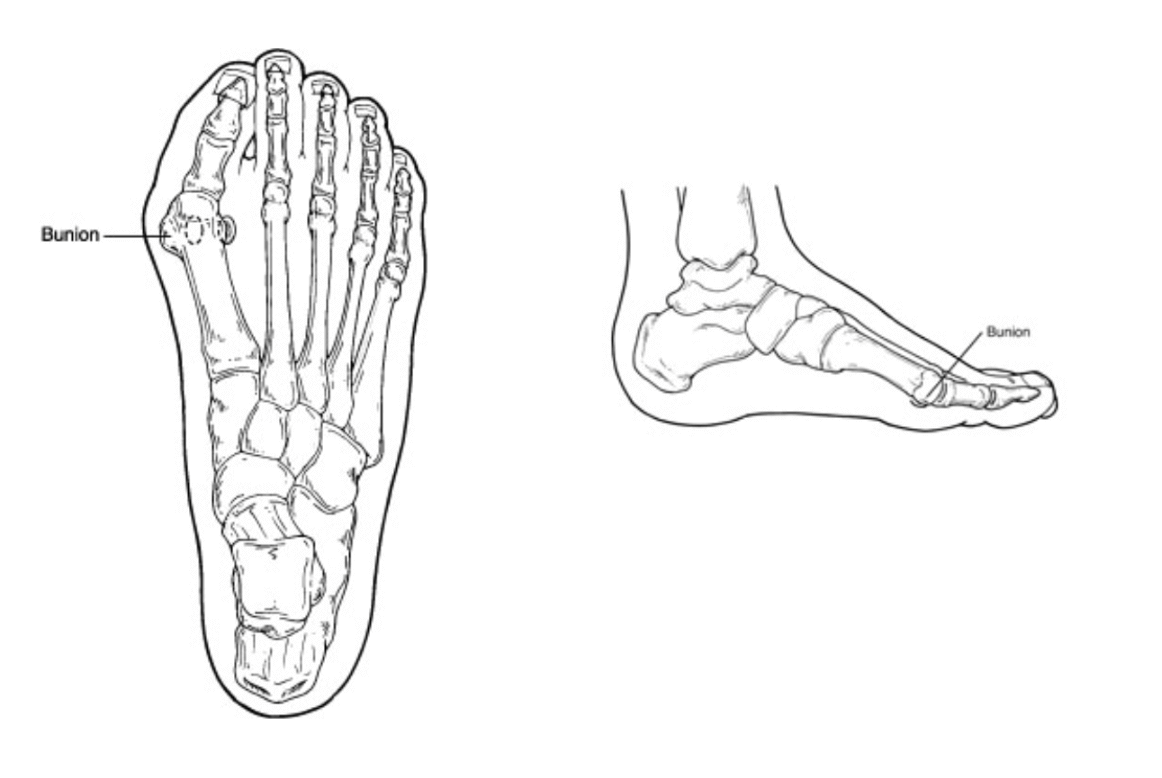
Bunions are painful deformities that are common and can cause pain and discomfort daily. Surgery for bunions has been around for over 100 years but recent advancements have made bunion surgery easier than ever. Today we will discuss the Lapiplasty bunion procedure, its advantages and how it has changed the way we correct bunions.
What is a bunion?
A bunion is an inherited foot issue that involves the deviation of a bone in your foot. Specifically the 1st metatarsal begins to drift in the wrong direction making it difficult to fit shoes and can be quite painful. Genetics play a big role in the development of a bunion and things like shoe gear can contribute to the bunion.
Convention bunion surgery often involves cutting the bone and realigning a joint. This type of procedure has been utilized for years and is still the most popular bunion surgery in the world. It has its applications and is appropriate for certain individuals. The Lapidus or Lapiplasty focuses on larger bunions and people that have a more unstable foot. It aims to correct the bunion in a more comprehensive approach and provides the best long term results.
It involves correcting the bunion in 3 planes, realigning the metatarsal, correcting the bunion at the root cause. The joint where the bunion originates is cut and realigned and fixated to heal in the proper position. Recovery can vary by patient and bone quality same with healing times. I do recommend physical therapy and follow up is essential.
In conclusion Lapiplasty has revolutionized bunion correction and provides excellent long term results and is by far the best procedure for many patients.
If you would like a consultation for your bunion I can help. Call to make an appointment with me at 425-391-8666 or make an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Dr. Brandon Nelson, A Board Certified Foot Physician & Surgeon, Issaquah’s Top Podiatrist, Discusses Heel Pain in Adults and Children

Heel pain can affect both adults and children alike. It is rare for it to be the same cause but does happen. Adults are more commonly inflicted with plantar fasciitis while children it is usually attributed to calcaneal apophysitis or Sever’s disease. The big difference is one is usually attributed to over use and the other growing pains. I will discuss both today.
Plantar fasciitis is still the most common reason people seek out a foot and ankle doctor. This presents with pain in the morning or after exercise. Typically it will get worse with time. There is sometimes a change in activity levels. I encourage you to be evaluated as soon as possible. This will decrease the course and make for a quicker recovery. Start at home with simple calf stretches and icing of the heel. Your doctor will give you a more formal program and usually heel pain resolves with conservative measures.
Heel pain in children is fairly common as well. The typical child is 10-14 years old and going through a growth spurt. You hear a lot about Sever’s disease when visiting the doctor’s office but there are a few outlying causes as well so a thorough workup is warranted. It usually begins with pain while walking or with sports. Again calf stretching and icing can go a long way.
If you have heel pain and want an evaluation schedule an appointment with me and I will help you.
Sincerely,
Board Certified Physician & Surgeon
Issaquah’s Top Podiatrist & Foot/Ankle Surgeon
Dr. Brandon Nelson, A Board Certified Foot Physician & Surgeon, Issaquah’s Top Podiatrist, Discusses the Best Bunion Procedure to Have

I have been practicing medicine now for about 15 years and like to look back from time to time on how it has changed. Currently there is a lot of talk about the Lapiplasty bunion and bunion surgery in general. I thought I would take a few minutes and discuss this topic.
Bunion surgery continues to be one of the most common foot surgeries in the United States if not the most common. I believe the last statistic I read was something like almost 350,000 operations per year. It is hard to believe there are that many bunions out there!
The most utilized bunion surgery is the Austin bunionectomy. This is for a couple reasons. One can correct the vast majority of bunions whether small or large. It has a much faster recovery and is technically not as challenging as other operations. It involves the cutting of the metatarsal head in a chevron pattern and shifting that bone medially. It is usually fixated in place with a few screws. Patients can bear weight immediately and are typically in a walking boot for 4-8 weeks. It has good long term results and will probably continue to be the most common bunionectomy for that reason.
The other most talked about bunion procedure is the Lapidus bunionectomy or the Lapiplasty. This procedure is the choice for very large bunions or juvenile bunions. It is technically more challenging but provides for excellent correction. This involves fusion of the metatarsal cuneiform joint to realign the metatarsal. It usually involves a period of non weight bearing from 3-8 weeks. The long term results are excellent.
That begs the question: which procedure is best for bunion patients? Well the answer is not simple. It really involves a couple key considerations. First being how does the rest of the foot look and how much motion do we have through the 1st metatarsal? Second is patient age and activity level. Third would be overall general health of the patient and bone quality. I recommend seeing a surgeon that performs a lot of bunion surgeries as their outcomes will be better.
If you have a bunion and would like to know your options and have it evaluated schedule, make an appointment with me and I will help you.
Sincerely,
Board Certified Physician & Surgeon
Issaquah’s Top Podiatrist & Foot/Ankle Surgeon
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Issaquah’s Best Podiatrist, Discusses Heel Pain

Heel pain can affect people of all ages, lifestyles and activity levels. You can be an avid exerciser, a home body or just spend all day working on your feet. I will discuss some of the causes of heel pain, the symptoms and when to seek medical attention. I have been a practicing podiatrist in Issaquah for over 25 years and have treated and helped 1000’s of patients.
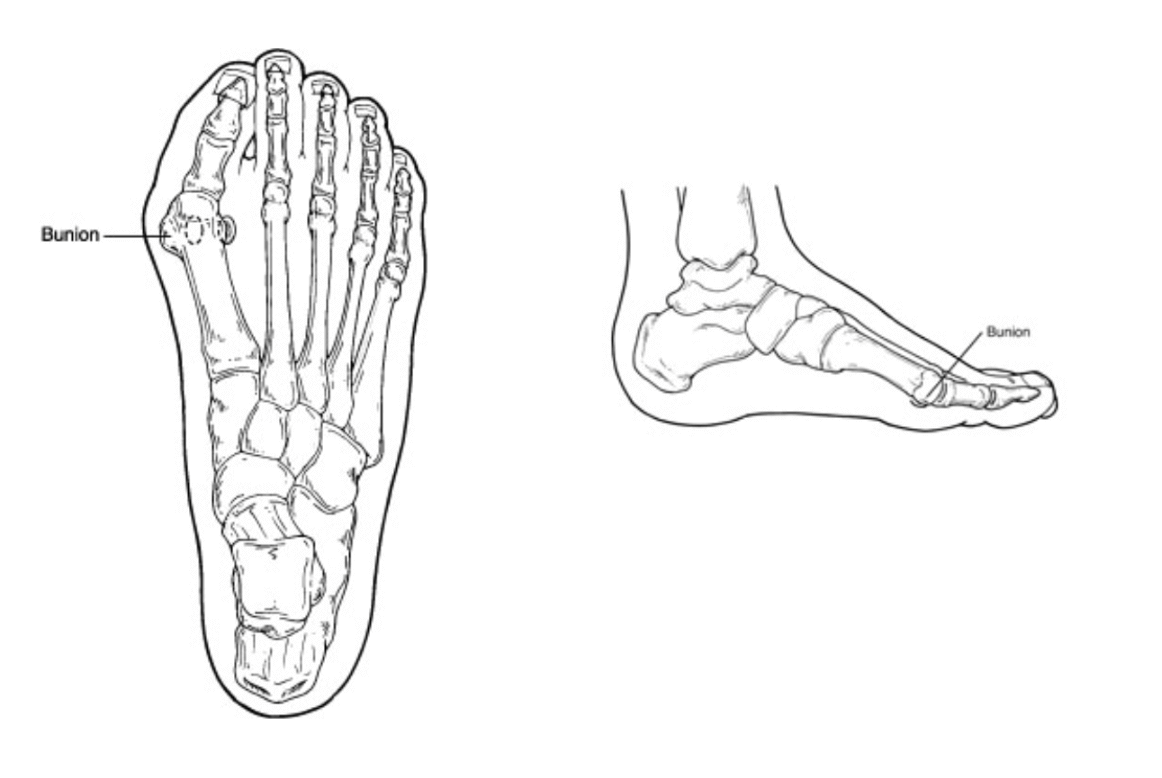
There are many common causes of heel pain. However a few are the most common and these include; plantar fasciitis, Achilles tendonitis, stress fractures and Baxter’s neuritis.
Plantar fasciitis is caused from an inflammation of a band of tissue running on the bottom of the foot. The job of the fascia is to support the arch of the foot and control 3 dimensional movement. It often occurs with repetitive stress like standing all day or running.
Achilles tendonitis is usually located more towards the back of the heel. The Achilles tendon helps to push off the foot during the gait cycle. Often any activity that increases load like jumping rope can cause the Achilles to become inflamed. People often feel swelling or a thickening of this tendon in the ankle.
Stress fractures are usually related to overtraining and time. They occur with repetitive loading of a bone. The bone I am speaking of in this case is the calcaneus. These can be tricky to diagnose.
Baxter’s neuritis is rare but is often confused for plantar fasciitis. There is usually more of a burning or tingling that occurs. Often there is not an increase in activities and no correlation with time spent on your feet and pain.
I recommend seeking early treatment for heel pain. I see that patients that wait longer have a harder time recovering and often need more therapeutic interventions. This is especially true for athletes, get in early and get a head of the pathology.
If you have heel pain and would like an appointment with Issaquah’s top Podiatrist at 425-391-8666 or make an appointment online.
Sincerely,
Board Certified Foot & Ankle Surgeon
Dr Brandon Nelson, A Board Certified Physician & Surgeon, Issaquah’s Best Podiatrist, Discusses Why Lapiplasty Bunion Correction
Bunion surgery is the most common foot surgery done in the United States. There are many different techniques to correct a bunion. Most involve either cutting of a bone or fusion of a bone. All involve realignment of a joint in order to improve the function and appearance of the foot.
I have now been practicing medicine and surgery for over 15 years. I am a podiatrist in Issaquah and have had the opportunity to help 1000’s of patients with bunions. Bunions can be extremely painful and the majority of people will require them to be fixed at some point. This experience has led me to utilize Lapiplasty on the majority of my patients.
Why the Lapiplasty?
1. It provides correction at the center of a bunion deformity
2. It has been proven to have the best long term outcomes
3. It stabilizes the foot structure
4. It does an excellent job for large bunions
5. It has been utilized for over 100 years
I encourage anybody with a bunion to get evaluated by a surgeon that performs a significant amount of bunion corrections annually. Experience can make a big difference in outcomes and the Lapiplasty is a technically difficult procedure to execute. If you have a bunion and would like to discuss the Lapiplasty make an appointment with Issaquah’s top Podiatrist at 425-391-8666 or make an online appointment.
Sincerely,
Board Certified Foot & Ankle Surgeon
Dr. Timothy Young discusses a different kind of bone spur in the foot: Enthesophytes, not your typical bone spur.

Dr. Timothy Young discusses a different kind of bone spur in the foot: Enthesophytes, not your typical bone spur.
Introduction:
There can be confusion when talking about bone spurs in the foot. In general, when one thinks of an arthritic bone spur, that is often an osteophyte. However, there is a different kind of bone spur; this is an enthesophyte. The best way to think of an enthesophyte is calcification of the tendon or ligament at its attachment to the bone. A common example would be a heel spur related to plantar fasciitis or calcification of the Achilles tendon where it attaches to the back of the heel bone. It is important to know, however, that calcification of the Achilles tendon or a plantar calcaneal heel spur, in either case, may not cause any pain or symptoms at all. On the other hand, if there is associated inflammation or degenerative changes, there may be symptoms and pain.
Enthesopathy is another similar term describing this condition. Note that Enthesopathy often occurs in response to a mechanical condition, but there can be more of a systemic inflammatory condition also, such as ankylosing spondylitis or psoriatic arthritis. Some of the autoimmune arthritic conditions may potentially be related to this condition.
Enthesophytes vs. Osteophytes: An Overview
Enthesophytes Defined: Enthesophytes are abnormal bony projections that occur at the attachment points of tendons or ligaments to the bone. These bony outgrowths are the result of the body's response to chronic stress and irritation in these connective tissues.
Osteophytes in Contrast: We have previously discussed osteophytes in our prior blog. Osteophytes are abnormal bony projections that form within joint spaces. Unlike enthesophytes, which are associated with the insertion points of tendons and ligaments, osteophytes develop as a response to joint degeneration and inflammation, often associated with conditions like osteoarthritis. The most common osteophytes in the foot and ankle could include the great toe joint, where bone spurs limit motion and cause an enlargement on the top of the joint. In the ankle, it is often the front of the ankle joint that develops osteophytes that can also limit ankle joint motion.
The Stress Response: Understanding Enthesophyte Formation
Chronic Tendon or Ligament Stress: Enthesophytes are born out of the repetitive stress and strain on tendons and ligaments. This stress can result from various factors, including overuse, improper biomechanics, or inflammatory conditions affecting the connective tissues.
Microtrauma and Inflammation: Microscopic damage to the tendon or ligament can lead to localized inflammation. As the body attempts to repair this damage, the bone responds by forming additional bony tissue at the insertion point – thus, an enthesophyte is born.
Common Locations: Enthesophytes can occur at multiple sites throughout the body. Common examples in the foot include the heel, with two common examples being Achilles enthesophyte and an enthesophyte associated with plantar fasciitis or the most typical heel spur.
Distinguishing Features: Enthesophytes vs. Osteophytes
Location:
Enthesophytes: Develop at the attachment sites of tendons or ligaments to bones.
Osteophytes: Form within joint spaces in response to joint degeneration.
Associations:
Enthesophytes: Linked to chronic tendon or ligament stress and inflammation.
Osteophytes: Associated with joint degeneration and conditions like osteoarthritis.
Clinical Manifestations:
Enthesophytes: May cause localized pain at the attachment sites, especially during movement.
Osteophytes: Can impact joint movement, causing pain, stiffness, and reduced range of motion.
Managing Enthesophytes: It is important to understand that in many cases, it is really because of the enthesopathy that we are treating so for calcification of the Achilles tendon, we often are treating Achilles tendon problems. And for treating a plantar calcaneal spur, we often are treating plantar fasciitis as the primary problem, and the enthesopathy may be a secondary problem.
Conservative Measures:
Rest, activity modification, and gradual return to exercise.
Physical Therapy: Stretching and strengthening exercises.
Anti-Inflammatory Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs) to manage inflammation and pain.
Orthotic Support:
Proper footwear and orthotic devices to alleviate stress on affected areas.
Shockwave Therapy: This is extremely effective at treating Achilles tendon problems and calcific Achilles insertional tendinosis and plantar fasciitis.
Platelet Treatments: Concentrated platelets are injected into the damaged tendon or plantar fascia.
Surgical Procedure Interventions:
Tenex: This is a less invasive type of procedure that can remove damaged tendon and remove some of the calcified portions.
Traditional Surgery: In resistant cases, surgical direct treatment may be considered.
Conclusion:
Enthesophytes may relate to the body's adaptation to the demands placed on tendons and ligaments. This condition may (or may not) cause discomfort, especially in the presence of chronic stress, and may limit exercise. Understanding their distinct nature and differentiating them from osteophytes is crucial for accurate diagnosis and effective management. If you suspect the presence of enthesophytes and experience persistent pain or discomfort, please contact our office for consultation or make an appointment online.
Dr Brandon Nelson, A Board-Certified Physician & Surgeon Discusses Why He Has Been Doing the Lapiplasty Procedure for over 15 years

Bunions are an inherited foot deformity that can be exasperated by shoe gear and activities. They are created when your first metatarsal begins to shift out of place to stabilize your foot. They usually become worse with time and eventually cause pain and discomfort. Many patients require surgical intervention.
The surgical correction of a bunion can have great outcomes and provide long lasting benefits. In the United States there are many different approaches to correction of a bunion. I have been operating long enough to have had experience in most of these procedures. That is why my bunion correction of choice is Lapidus or Lapiplasty.
The Lapidus or Lapiplasty is a procedure that dates back almost 100 years. It was first described by Dr Lapidus and to date has stood the test of time for bunion correction. It involves utilizing a fusion of 2 bones at the apex of the bunion or where the bunion starts. This provides dynamic correction and great long-term stability. I find patients are happy with their new foot structure and often want the other side fixed as well.
If you have been contemplating bunion surgery, give me a call. I have an onsite surgery center that saves time and money. IV sedation provides for a great experience. If you would like a consultation for your bunion I can help. Call to make an appointment with me at 425-391-8666 or make an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons