A
abductor (muscle)
achillobursitis
aclasis – pathological continuity of structure
acrodermatitis enteropathica
acrokeratosis paraneoplastica – Bazex syndrome
adductor (muscle)
adiposis dolorosa – Dercum disease
aDWF – ankle Doppler wave form
AFO – ankle-foot orthosis
alligator skin – ichthyosis congenita
allylamines – e.g. Naftin (naftifine)
angle, DMMA – distal metatarsal articular, Engel, Fowler-Philip, Kite, talo-first, Taygar
ankylosis
anserinoplasty
antalgic gait
AOFS hindfoot ankle score
apophysitis
aPVR – ankle pulse volume recording
atavistic tarsometatarsal joint
athlete’s foot – tinea pedis, ringworm of the feet
atavism
PROPER NOUNS:
Abrikosoff tumor
Alizarin sweat test
Allen maneuver
Apelqvist grades 1 through 4
Ashurst-Bromer classification of ankle fracture
Atasoy flap for nail injury repair
Austin – bunionectomy, screw, wire
B
ball-and-ring device
basal cell nevus syndrome
basic fuchsin (in fungicides)
BB – blunted and bowed
bipivotal hinge
bivalve of cast
BK amputation/case – below-the-knee
blebs
bowing of bone
bowleg; bowlegged – genu valgum
brachymetatarsia
bubble patch
bunion (see proper names in second alpha section)
bunionectomy
bunionette
bursitis – inflammation of the bursa of a joint
bursotomy
butenafine hydrochloride – Mentax (antifungal)
PROPER NOUNS:
Banks-Laufman incision
Bannon-Klein implant
Bardenheuer bifurcation procedure
Bart-Phumphery syndrome
Bazex syndrome – acrokeratosis paraneoplastica
Beau lines
Bechtol arthroplasty
Bednar tumor
Berman-Gartland procedure
Betadine scrub
Bier amputation
Blair arthrodesis
Blajwas-Schwartz-Marcinko irrigation/drainage system
Bledsoe cast brace
Blex contractile force curve
Blount, brace, disease, staples
Blucher opening
Bodsky ischemia classification
Boots: Acme, Denis Browne, Dingo, Gibney, 9-West, Red Dog, SACH, Sorel, Stride Rite,
Technica, TheraBoot, Unna Gelcast/gelatin, Unna paste, Vasque
Brace, dropfoot, (AFO), ischial weightbearing, Knight, Lyman-Smith, Milwaukee,
Stabheilizer (for footdrop), Taylor, toe drop, weightbearing
Brewster triple arthrodesis
Brockman incision
Brostrom procedure
Bunion – hallux abductovalgus, last, tailor’s,
Bunionectomy:
Akin
Austin
Joplin
Keller
Kreuscher
Lapidus
Logriscino
McBride
Mitchell
Reverdin
scarf osteotomy
Silver
Stone
tricorrectional
Wu
Z
Brunnstrom stage I-V
Bunnell, anvil, drill, needle, operation, probe
Burns-Haney incision
Burow triangle
C
calcaneal – pertaining to the calcaneus bone
calcaneitis
calcaneoapohysitis
calcaneoastragaloid
calcaneocavus
calcaneocuboid
calcanodynia
calcaneofibular
calcaneonavicular
calcaneoplantar
calcaneoscaphoid
calcaneotibial
calcaneovalgocavus
calcaneus bone
calcar, femorale, pedis
calcarine
calf-corset weightbearing
calf-lacing, double-upright brace
callosity – pertaining to a callus
callus; calluses
capillary refill (time)
capsulitis
cast brace/boot
castaway orthotic
CCE – clubbing, cyanosis, edema
cellulitis
cetylpyridinium Cl
cheiropodalgia
chemical matricectomy
chevron osteotomy
chloroxylenol
chondroma – tumor of the chondral tissue
clam, clamshell walker
claudication
clavus, clavi: corn, heloma, duras, hystericus, interdigital, mollis, secalinus
clawfoot
clawtoe(s)
cleft foot
clonus; ankle, toe
clubfoot – see talipes
coalition
cookie; metatarsal c.
coralline hydroxyapatite
corn – clavus, hard, interdigital, kissing, soft
counter of shoe
coax, valga/varum
crescentic osteotomy
CRPS – chronic regional pain syndrome
PROPER NOUNS:
Calandruccio fixation device
Cam Walker walking brace
Can-Am brace
Carville sandal
Cam Walker CBWO screw
Chambers osteotomy
Chang-Miltner incision
Charcot, arthrosis, foot, joint, restraint, procedure disease
C. restraint orthosis walker
Charcot-Marie-Tooth disease – CMT
Charnley, arthrodesis, fixator
Charnley-Mueller; arthroplasty/prosthesis
Chopart amputation
Chrisman-Snook ankle reconstruction
Cincinnati incision
Clayton procedure
Clearz – a fungicide
Coban dressing
Cobbies shoewear
Codman triangle
Cole osteotomy for midfoot deformity
Coleman block test
Colonna-Ralston incision
Comf-Orthotic insoles
Converse athletic shoewear
Comed footgear
Compound W
Cook walking brace
Corfan shoe
Cotrel-Dubousset brace
Count’R-Force arch brace
Couvelaire incision
Crego elevator
CROW brace
CRPS – chronic regional pain syndrome
Cryo Cuff
Curtain incision
Cutter implant
Cymeline
D
danglefoot, aka dropfoot
DCCT – Diabetes Control and Complications Trial
decubitus ulcer
dendritic synovitis
desquamates
DFO – dorsiflexion osteotomy
dial-in cut osteotomy
diabetic toe(s)-(foot or feet) – see ULCER
diaphysis
DIP joint; DIPJ – distal interphalangeal joint
disk disease
DMMA – distal metatarsal articular angle
dorsomedial
duckfooted – flatfooted
duckwalk
duck waddle
PROPER NOUNS:
Danis-Weber classification of ankle injury
DarcoGel ankle brace
Darier sign
De Guglielmo disease – erythemic myelosis
De Morgan spots
Dejerine-Sottas disease
Denis Browne, bar, boot, splint, shoe
Dercum disease
DesignLine orthotic
Diab-A-Thotics
Di Guglielmo disease – erythemic myelosis
Dias-Tachdjian classification of physeal injury
Dickinson approach
Diebold-Bejjani osteotomy
Di Guglielmo disease
Donjoy RocketSoc ankle brace
Downey-McGlamry procedure
Dressflex orthotic
Dr. Scholl’s foot products
Dubreuilh melanosis circumscripta
Dunn triple arthrodesis
DuoFilm products
Dupuytren, contracture, exostosis
DuVries incision/repair
Dwyer osteotomy
Dynafo ankle-foot orthosis (or D. AFO)
Dynasplint orthotics
DynaStep
E
epiphysis, epiphyseal
PROPER NOUNS:
Eastersohn osteotomy for tailor’s bunion
Easy Spirit shoewear
Eaton-Lambert syndrome
Eckert-Davis classification of peroneal tendon subluxation
Eichenholtz stage
Elastomull
Elmslie procedure
Engel angle
Esmarch bandage/tourniquet
Essex-Lopresti fracture
Etonic shoes
Evans calcaneal osteotomy
Evazote
F
flaccid
flatfoot
flexion/extension
fractures – (see list in Surgical Compendium)
fungus
PROPER NOUNS:
Famolare shoes
Farber disease
Felty syndrome
Flex Foot products
Floam cushion
Florsheim shoes
Footmaxx orthotics
Foot Medic products
Forestier disease
Fosnaugh nail biopsy
Fowler-Philip angle
Freer elevation
Freiberg infraction (not infarction)
Friedreich
Forst H-block
Fungus products: Fungatin, Fungi Clear, Fungi-Nail – sorcinol, salicylic acid
G
GAIT, antalgic, ataxic, gegenhalten, halting, spastic, scissor, three-point, Trendelenburg, two-point
ganglion cyst
gastrocnemius
gastrocsoleus
GENU – knee, recurvatum, varum – bowleg, valgus/valgum – knock knee
gout – podagra; tophaceous. gouty arthropathy
gun-barrel sign
guttate keratoses
PROPER NOUNS:
Ganley splint
Gowers sign
H
hammertoe(s)
hamstring muscle/tendon
HALLUX, dolorosa, flexus, limitus (limitans), malleus, rigidus, valgus, interphalangeus –HBO – hyperbaric oxygen therapy (baro chamber)
healing sandal
heloma
helosis
helotomy
hemi-implant
hindfoot
PROPER NOUNS:
Hawkins classification of talar fractures
Homan sign/test
I
intoeing gait
iontophoresis
IPJ – interphalangeal joint; DIPJ, PIPJ
J
JERK, Achilles, ankle, quadriceps, triceps, surae
PROPER NOUNS:
Jahss classification of MTPJ dislocation
K
keratoderma
keratoma
keratosis
knock-knee – genu varum
koilonychia – spoon nail
L
leg-length discrepancy
PROPER NOUNS:
Lachman sign/test
Langer arch, lines
Lauge-Hansen classification of ankle fracture
Leser-Trelat sign
Lhermitte sign/symptom
Litecast
Low Dye strap/tape
Luir-Torre syndrome
M
matrix; matrices
metatarsalgia
metatarsocunieform
mortise
PROPER NOUNS:
Mediplast plaster – salicylic acid
Mees lines
Mephisto orthotic shoes
Morton neuroma
Mulder sign
N
NAIL, nailbed, matrix, parrot beak, reedy, spoon, turtleback, watch-crystal
neoprene ankle support/brace
neuralgia
neuritis, peripheral
nonweightbearing
O
onychia
orthotic device; orthotics
orthotist
os, calcis
osteochondroma
osteotomy
PROPER NOUNS:
Ogden classification of epiphyseal fractures
Ohashiatsu foot massage, shiatsu
P
paronychia, perionychia – herpetic, tendinosa
pemphigus
PES, (pedes), abductus, adductus, anserinus, arcuatus, calcaneus, carinatum, cavus, equinovalgus, equinovarus, equines, febricitans, gigas, planovalgus, planus, pronatus, supinatus
PFMT osteotomy
phalanx; phalanges
pilon (tibial)
PIP joint – proximal interphalangeal joint
piriformis
plafond – tibial pilon
planovalgus
PLANTAR, callosities, fasciitis, fibroma, tyloma, warts – verruca plantaris/verruca pedis
plantaris – plantar; sole
plantigrade
PNP – peroneal nerve palsy (footdrop)
podagra – gout
podalgia
popliteus
pouce flottant – ray defect
PPG – photoplethysmography
pronation/supination
prop-and-press device
proximal interphalangeal joint – PIPJ
psoriasis
pterygia of nails (singular – pterygium)
PROPER NOUNS:
PLA screws – polyactide absorbable screws
Q
quick – (the flesh at the leading edge of a fingernail or toenail)
R
ray – digit, toe/finger
rearfoot
retrocalcaneobursitis (or retrocalcaneal bursitis)
rockerbottom foot
rubor
PROPER NOUNS:
Rosenthal classification of nail injuries
S
sartorius
sciatica
scleroderma
Seattle foot
semimembranosus
semitendinosus
sesamoid bones
sesamoiditis
spur, calcaneal s.
STOCKING, dysesthesia, TED hose
subtalar joint
subtarsal
supination/pronation
suture – (see list in Surgical Compendium)
syndactyly
syndesmosis tibiofibularis
synovial cyst
PROPER NOUNS:
Salter-Harris classification of epiphyseal fractures
Supp Hose
Sudeck a.SD3 stirrup brace
SWMF – Semmes-Weinstein 10-gm monofilament
T
talipes, clubfoot
talus, talar
tarsonavicular bone
tarsal tunnel syndrome
tenalgia
tendo (pl: tendines)
tendo calcaneus
tendo Achillis (Achilles tendon)
tendon – see MUSCLES AND TENDONS
tendon enthesis (junction of tendon and bone)
tendon of Hector
tendon washer
tendinitis
tendinoplasty
tendinous
tensor fasciae latae
tenodesis
tenolysis
tenosynovitis
TENS unit (Transcutaneous Electrostimulator)
tibia vara – Blount disease
tibial pilon – plafond
tibial torsion
tibialis anticus (anterior)
tibialis posticus (posterior)
TINEA, athlete’s foot (pedis), cruris, manus, transversalis
TRIANGLE, Burow t., Odman, Kager
triceps surae (sural muscle)
triple arthrodesis
tyloma – callus, (corn), tyloma mollum, tylosis plantaris, tylotic, tyroid (cheesy)
PROPER NOUNS:
Taygar angle
Taylor brace/splint
TBI – toe:brachial index
TBSA – total body surface area
TcPO2 (or) TcpO2, etc. – transcutaneous partial pressure oxygen
TED – thromboembolic disease
TED hose/stockings
Thurston Holland flag sign
Tscherne-Gotzen classification of tibial fractures
U
ULCER, decubitus, diabetic (toe/s, foot/feet), full-thickness, ischemic, partial-thickness, pressure, venous stasis
ungual tuft, unguis, ungues, unguis incarnates, unguis matrix
PROPER NOUNS:
UNNA (Unna), flex compression dressing, Gelcast, gelatin boot, wrap
V
VAE – venous air embolism
valgus, valga, valgum, coax, genu, talpies, valgus rotation
vallum unguis
varicosity
varix
varus, varum, same as valgus
vastus – intermedius, lateralis, medialis (internus)
VEGF – vascular endothelial growth factor
VERRUCA, verrucae (wart), acuminate, condyloma acuminatum, digitata, filiformis
necrogenica, peruana, peruviana, plana, plana juvenilis, plantaris – plantar wart,
seborrheica – seborrheic keratosis
verrucose
verrucosis
verrucous
PROPER NOUNS:
Velcro
Verocay bodies
W
wart – verruca
web space
weightbearing; nonweightbearing
PROPER NOUNS:
WIRE, Kirschner AKA K-wire, Kerrison, titanium
Wolff law (regarding bone structure)
X – NO REFERENCES
Y – NO REFERENCES
Z
PROPER NOUNS
Zymderm collagen implant
 There are several causes of pain in the ball of the foot. The type of pain and its location help the doctor in determining the cause of the pain and helps to direct them in the best treatment for the patient.
There are several causes of pain in the ball of the foot. The type of pain and its location help the doctor in determining the cause of the pain and helps to direct them in the best treatment for the patient. 

 Flatfoot is often a complex disorder, with diverse symptoms and varying degrees of deformity and disability. There are several types of flatfoot, all of which have one characteristic in common: partial or total collapse (loss) of the arch.
Flatfoot is often a complex disorder, with diverse symptoms and varying degrees of deformity and disability. There are several types of flatfoot, all of which have one characteristic in common: partial or total collapse (loss) of the arch.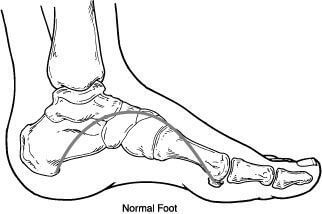 Flexible flatfoot is one of the most common types of flatfoot. It typically begins in childhood or adolescence and continues into adulthood. It usually occurs in both feet and progresses in severity throughout the adult years. As the deformity worsens, the soft tissues (tendons and ligaments) of the arch may stretch or tear and can become inflamed.
Flexible flatfoot is one of the most common types of flatfoot. It typically begins in childhood or adolescence and continues into adulthood. It usually occurs in both feet and progresses in severity throughout the adult years. As the deformity worsens, the soft tissues (tendons and ligaments) of the arch may stretch or tear and can become inflamed.
