When plantar fasciitis is causing heel pain, grab some juice and take a break.
Now, apply the juice directly to your foot...
If relief is what you are after and would like to try to ease the pain at home, try frozen juice.
Juice concentrates come in a cylindrical container that will easily roll along the bottom of your foot. When your plantar fasciitis is causing pain, take a frozen juice concentrate. Right out of the freezer it may be too cold, so you may want to place a towel over the container. This will create a barrier so that the frozen juice container does not add to any discomfort.
Before placing your foot on top of a frozen juice container check to see that it is sealed and do not apply too much pressure. The safety of your juice container and the floor below are at stake here. If the container is not sealed or is punctured you will likely have a sticky mess.
From a seated position you will gently roll the frozen juice container along the arch of your foot to your heel and back again. A few minutes of this can provide some relief to the pain associated with plantar fasciitis.
Heel pain that does not subside should be evaluated by a doctor. If you find that you are limping in the morning, when you first get out of bed, plantar fasciitis is the likely cause. Read more about the causes, diagnosis and treatment options for plantar fasciitis.
After rolling your feet over the juice concentrate you can easily mix up a beverage to enjoy and relax. Resting the painful plantar fascia is important. When the plantar fascia becomes irritated, inflamed or torn, it requires down time to heal. If possible try spending a little more time with your feet up and less of any activities that may have caused the strain of your plantar fascia.
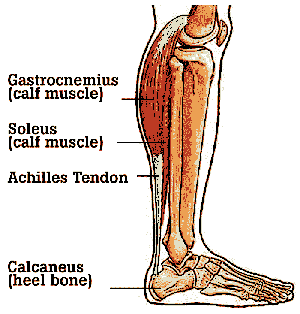
The plantar fascia is the thick ligament that connects your heel to your toes and is one of the most common causes of heel pain. Some of the common causes of this condition are a high arch, wearing high heeled shoes, running or being overweight. A tight Achilles tendon can also be to blame. Because of this stretching your calf muscles can relieve tension on your plantar fascia.
When the heel pain is frequent and nagging it is time to see a doctor. One common approach is to treat this type of heel pain is with prescription orthotics. Depending upon the severity of the injury (plantar fasciitis is generally caused by overuse, that causes strain and tearing of the plantar fascia) there are many treatment options. Surgery for plantar fasciitis is often the last resort.





 What is it?
What is it?






 The plantar fascia spans from the heel to the forefoot and extends into the base of the toes. The calf muscle, including the gastrocnemius and soleus muscles, combine and attach at the heel to form the Achilles tendon. The soleus muscle attaches to the tibia and fibula below the knee and the gastrocnemius muscle extends and attaches above-the-knee.
The plantar fascia spans from the heel to the forefoot and extends into the base of the toes. The calf muscle, including the gastrocnemius and soleus muscles, combine and attach at the heel to form the Achilles tendon. The soleus muscle attaches to the tibia and fibula below the knee and the gastrocnemius muscle extends and attaches above-the-knee.