First metatarsal neck osteotomies are known by various names based on the individual who first described the procedure (e.g. Austin, Reverdin-Green, Kalish-Austin). Regardless of the procedure, the goal of all these procedures is the same, to remove the bump and realign the joint. The first part of all bunion procedures involves removing the bump of bone from the side of the 1st metatarsal head. This is performed in a manner so as not to damage the viable part of the joint and not to leave any irregularities of bone that can cause future irritation in shoes. Once this is completed, the podiatric surgeon will create an osteotomy (bone cut) through the first metatarsal that will allow shifting the bone and realigning the joint. Depending on the type of osteotomy, the actual shape of the bone cut can vary. In the case of the Austin bunionectomy, the bone cut is V-shaped with the "V" sitting on its side and the tip of the "V" pointing toward the joint. When this cut is completed, the head of the metatarsal and joint is shifted toward the 2nd toe. In this way the bone and joint are repositioned in a more normal position. The Reverdin-Green osteotomy is made in a similar location but is trapezoidal in shape rather than V-shaped. Both these procedures are stable bone cuts and provide good correction of mild to moderate deformities. The Kalish-Austin bunionectomy is a modification of the Austin bunionectomy. It also is a V-shaped bone cut but is typically used for greater degrees of bunion deformities.
Because bone is cut and repositioned, it is often preferred to fixate or hold the bone in place with some external device. In the case of the Austin and Reverdin-Green osteotomies, this is most often accomplished by the use of a stainless steel pin across the bone cut. This prevents accidental displacement and loss of correction. Over the past 5 years, it has become increasing more advantageous to use small stainless steel or titanium screws to provide compression of the bone and to hold the bone in position. This is the main advantage of the Kalish-Austin bunionectomy. By using the screws, bone will heal faster and will allow for earlier ambulation. The screws are typically left in permanently unless they cause irritation of the soft tissues while the pins are generally removed in the office setting in three to four weeks following the day of surgery. The surgery is generally preformed as an outpatient in a hospital or out patient surgery center. Anesthesia is the choice of the surgeon made in consultation with the patient and anesthesiologist. Anesthesia may be a general anesthesia, twilight anesthesia or a local anesthesia.
Post Operative Care
The postoperative course and rehabilitation following bunion surgery depends on the procedure and can vary amongst podiatric surgeons. Patients have varying levels of postoperative pain but quite often the pain is significantly less than what the patient anticipates. A period of total non-weight bearing with crutches may be recommended in the first 3 to 5 days. In many instances, the surgeon may allow the patient to bear full weight in a postoperative surgical shoe. In all cases patients are instructed to limit their activities and to elevate their feet above their heart during the first 3 to 5 days. After this, a resumption of gradual weight bearing with a special surgical shoe is begun. Walking without the postoperative shoe is strictly prohibited. In cases where a pin is used, return to full weight bearing with a stiff soled walking shoe is allowed after the pin has been removed, generally in 3 to 4 weeks following the bunion surgery. Screws provide increased stability when used to fixate bone cuts and most patients can return to full weight bearing and regular shoes in 3-4 weeks following the surgery. The postoperative and rehabilitative course is improved by the use of ice and elevation of the extremity as much as possible. One of the most important aspects of the postoperative treatment is early motion of the joint to prevent joint stiffness. In most cases, range of motion exercises are begun almost immediately following surgery. No matter what the form of bone fixation is used, pins or screws; bone healing will take 6 to 8 weeks or longer. During this period of time it is important that the patient not walk without shoes or in thin-soled shoes or sandals. Should the patient risk walking without an adequately supportive shoe, they risk re-fracturing the bone and increase the duration of healing.
Possible Complications
Complications following bunion surgery are uncommon but may include infection, suture reaction, delayed or nonunion of the osteotomy, irritation from the pin or screws, stiff joint or recurrence of the deformity. Recurrence of the deformity can be halted or slowed with the use of functional foot orthotics. It is important to realize that surgery does not correct the cause of the bunion deformity. Functional foot orthotics however do address the cause of the deformity and their use are strongly encouraged following bunion surgery. A rare complication is the over correction of the bunion deformity. This condition, called Hallux Varus, may require additional surgery for its correction
This article should serve as a guideline for patients who are contemplating bunion surgery. The most commonly performed procedures for treatment of bunions have been discussed here. Procedures are selected based on surgeon's experience and preference. Patients are encouraged to discuss the surgery, the postoperative course and possible complications with their podiatric surgeon openly before consenting to surgical intervention.
| Glossary of Terms | ||
| Bunion | Bump on the side of the foot at the base of the great toe | |
| Bursitis | An inflammation of a fluid sac often found overlying a bunion | |
| Fixation | Act of holding bones together, commonly require external devices such as pins, screws or plates | |
| Hallux abductovalgus (HAV) | Medical term describing the deviation of the great toe toward the 2nd toe; common component of bunions | |
| Metatarsal | A long bone of the foot that forms the ball of the foot | |
| Orthoses | Devices made from a mold of the foot used to control abnormal motion of the foot; may be prescribed to prevent progression of bunion deformity or reoccurance following bunion surgery | |
| Osteotomy | Surgical procedure that creates a cut in a bone to achieve realignment; a "surgical fracture" | |
| Pronation | Motion of the foot which when excessive results in flattening of the arch; one possible cause of bunion formation | |
| Toe box | Part of the shoe that covers the toes | |
About the Authors:
Kenneth W. Oglesby, D.P.M., Second-year podiatric surgical resident, Beth Israel Deaconess Medical Center, Boston, Mass.
John M. Giurini, D.P.M., Chief, Division of Podiatry, Beth Israel Deaconess Medical Center, Boston, Mass., Assistant Clinical Professor of surgery, Harvard Medical School, Boston, Mass.




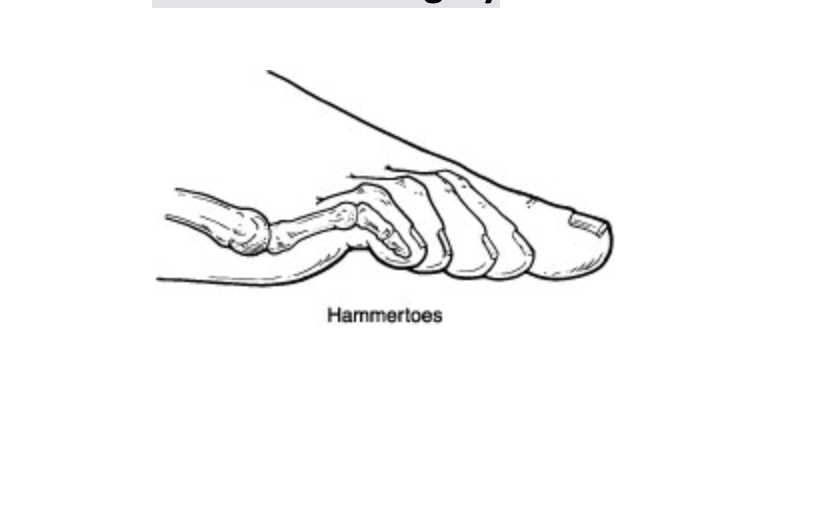 Hammertoes occur from contracture normally of the interphalangeal joints of the toes. These can occur in conjunction with other types of foot deformities like bunions or flat feet. These are fairly straightforward to fix surgically and have a very short recovery. One of the most important things I can encourage is to make sure other foot deformities are evaluated and treated. Normally the surgical procedure involves removing a small section of bone and pinning the toe for about 4 weeks. Most people are walking usually in a boot to protect the toes and physical therapy is not normally required. At the Bellevue foot surgery Center this procedure can normally performed and less than half an hour people often go back to work the next day. There are additional options for patients that don’t want third toes pinned, we continues internal splinting. Hammertoe deformity and wanted to discuss either conservative or surgical care we would be happy to review your options. If you live in Issaquah, Bellevue, Seattle, Redmond, Sammamish, Maple Valley and Renton please call us at 425–391–8666.
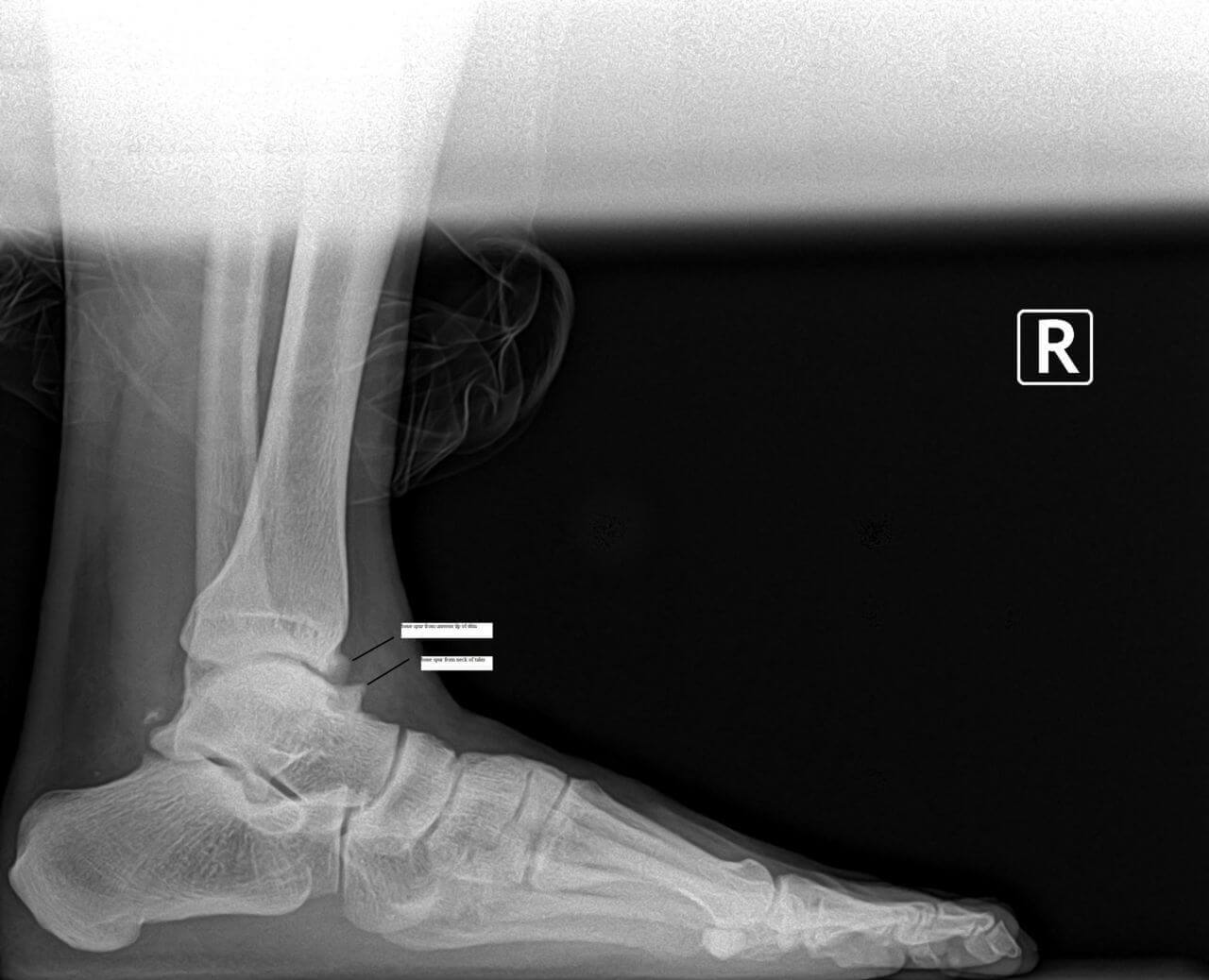
Hammertoes occur from contracture normally of the interphalangeal joints of the toes. These can occur in conjunction with other types of foot deformities like bunions or flat feet. These are fairly straightforward to fix surgically and have a very short recovery. One of the most important things I can encourage is to make sure other foot deformities are evaluated and treated. Normally the surgical procedure involves removing a small section of bone and pinning the toe for about 4 weeks. Most people are walking usually in a boot to protect the toes and physical therapy is not normally required. At the Bellevue foot surgery Center this procedure can normally performed and less than half an hour people often go back to work the next day. There are additional options for patients that don’t want third toes pinned, we continues internal splinting. Hammertoe deformity and wanted to discuss either conservative or surgical care we would be happy to review your options. If you live in Issaquah, Bellevue, Seattle, Redmond, Sammamish, Maple Valley and Renton please call us at 425–391–8666.  Pain and swelling around the joint is often indicative of arthritis. There are many treatment options available for arthritis including bracing, injections and surgery. Today I’ll focus on arthritis of the great toe joint or the first MTPJ. This is a chronic condition we see often described as hallux limitus or hallux rigidus. Many times patients have had injuries like turf toe or spraining of the toe joint, however this can be genetic as well. Usually pain presents with activities and often limits patient’s ability to play sports or running. Proper evaluation usually involves an x-ray see x-ray below was a good example of arthritis of the big toe joint.
Pain and swelling around the joint is often indicative of arthritis. There are many treatment options available for arthritis including bracing, injections and surgery. Today I’ll focus on arthritis of the great toe joint or the first MTPJ. This is a chronic condition we see often described as hallux limitus or hallux rigidus. Many times patients have had injuries like turf toe or spraining of the toe joint, however this can be genetic as well. Usually pain presents with activities and often limits patient’s ability to play sports or running. Proper evaluation usually involves an x-ray see x-ray below was a good example of arthritis of the big toe joint.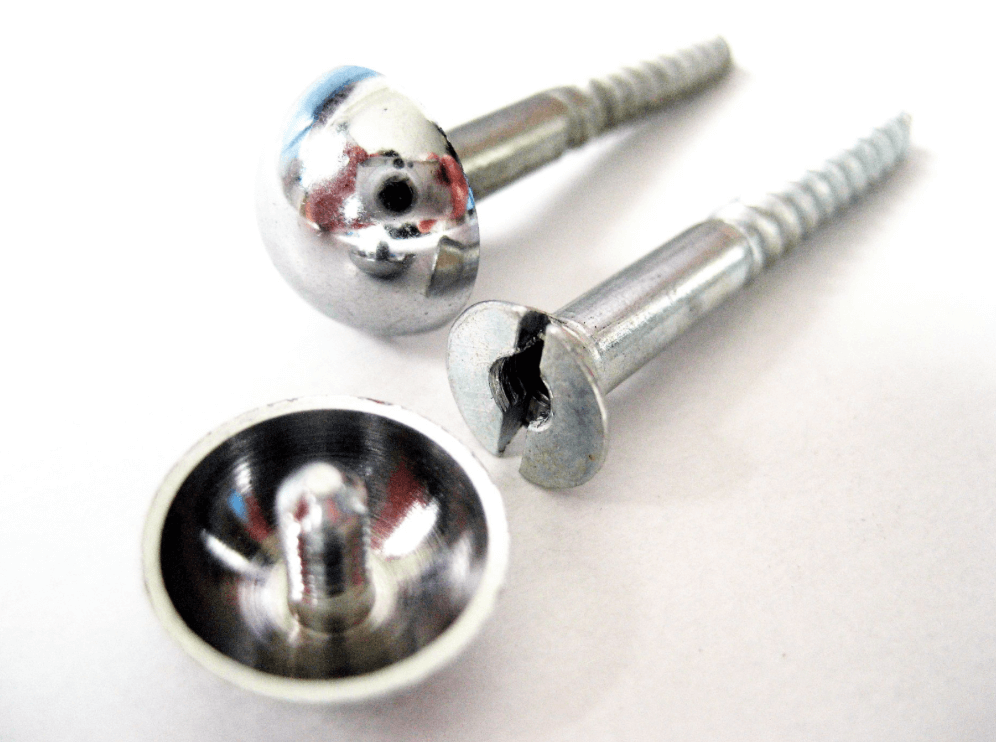 We have quite a few patients who’ve expressed interest in the removal screws and plates and/or pins. They’ve previously had surgery and would like their hardware taken out, often times because of irritation. Generally there appears to be an inflammatory-type reaction that some people experience from the retained hardware. Hardware removal is a very simple procedure that can be done in our surgery center oftentimes in less than 30 minutes. There’s usually hardly any recovery time, including minimal time off work if not just the day of surgery. Postoperative pain is often not present. We have very few people take any pain medication after this hardware removal. A common question patients have concerns the hole left behind by the hardware. Normally, new bone formation covers the hole in a relatively short period of time. If you have any questions about hardware removal or would like to be evaluated for hardware removal, please feel free to contact us at 425-391-8666.
We have quite a few patients who’ve expressed interest in the removal screws and plates and/or pins. They’ve previously had surgery and would like their hardware taken out, often times because of irritation. Generally there appears to be an inflammatory-type reaction that some people experience from the retained hardware. Hardware removal is a very simple procedure that can be done in our surgery center oftentimes in less than 30 minutes. There’s usually hardly any recovery time, including minimal time off work if not just the day of surgery. Postoperative pain is often not present. We have very few people take any pain medication after this hardware removal. A common question patients have concerns the hole left behind by the hardware. Normally, new bone formation covers the hole in a relatively short period of time. If you have any questions about hardware removal or would like to be evaluated for hardware removal, please feel free to contact us at 425-391-8666.