The ankle joint consists of portions of three bones: the talar dome, distal tibial plafond and distal fibula. The talus and tibia portions make up over 80% of the articular surface area of the ankle joint. Arthrodesis procedures are the removal of cartilage and any diseased bone from a joint to produce a fusion of at least two bones to create one bone. This removal of cartilage exposes the underlying bone on both sides of the joint. These joints surfaces are then compressed together with some form of fixation to create the fusion. In an ankle arthrodesis, typically the tibial position is fused to the talus. In some cases the fibula is part of arthrodesis, but this is the surgeon’s preference.
Why is an ankle arthrodesis procedure performed?
Ankle arthrodesis procedures are typically performed when all conservative options have been attempted and failed. Some of these treatment options, are corticosteroid injections, ankle foot orthoses, anti-inflammatory medications, custom orthotics, ankle braces, and sometimes arthrotomy or arthroscopy. In cases where the pain and/or the deformity is unremitting the arthrodesis is recommended. Some of the conditions that produce unremitting pain and deformity in the ankle joint are:
- Post-traumatic arthritis
- Rheumatoid arthritis
- Infection
- Failed ankle implant
- Congenital ankle deformities
- Neuromuscular disorders (i.e. post-polio syndrome, paraplegia, etc.)
- Lateral ankle instability (after failure of operative and non-operative treatment)
- Avascular Necrosis (secondary to trauma or metabolic disease states)
- Charcot Neuropathy
Techniques for ankle arthrodesis
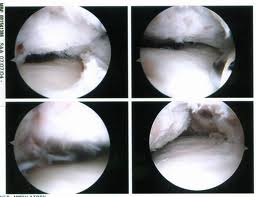
Over the years many techniques have been devised to fuse the ankle joint. Today there are three different techniques that your surgeon may use. They are open technique (use of one or two incisions on the outside and the front of your ankle) with screw fixation, open technique with external fixator fixation and arthroscopic ankle arthrodesis. Most surgeons use all three of these techniques, with the open technique with screw fixation the most commonly used. The technique used is surgeon's preference for your clinical findings, but all have equal fusion rates. Sometimes your doctor may need the use of bone graft, typically taken from your hip area (iliac crest), if you have defects in you ankle from previous trauma or surgery to help support the arthrodesis site.
What to Expect Following the Procedure
After most ankle arthrodesis procedures, your surgeon will have you non-weightbearing (no weight on your foot) typically for a period of 6-12 weeks, but this can be extended longer if there is any delay in healing of the arthrodesis site. After the surgery, you will be in a below knee cast or splint to help protect the surgical site and also prevent any movement. After the 6-12 weeks period your surgeon, will typically start you partially weightbearing with your crutches with the use of some type of cast or ankle brace for 4-6 weeks. Once you are fully weightbearing in the cast brace, you will be progressed into high-topped shoe or sneaker. Sometimes modifications have to be made to your shoes, called a rocker-bottomed sole, to aid in push off in ambulation after surgery.
Some other things that are important to note after the surgery, typically there will be some level of pain or discomfort after the surgery. In a majority of cases, you will be admitted after the surgery to the hospital for pain management. This admission can range from 23 hour to 3-4 days based on an individual’s pain tolerance. When in the hospital and also when you go home it is essential that you keep your foot elevated and use ice as recommended by your surgeon. Ice and elevation will help to reduce the swelling around your foot and ankle that is common after a major surgical reconstruction. The swelling in your foot and ankle can last for 6-9 months and even up to a year. Another thing that is tied closely to the swelling after surgery is a phenomenon that occurs when you get up from after you have had your foot elevated for a period of time. What happens is when you dangle your leg to get up, blood flow will increase into the foot and ankle which will create a throbbing sensation and sometimes a pins and needles sensation in your foot. This is perfectly normal and will go away when you re-elevate your foot.
Recovery Time
Time off work depends on the type of ones work as well as the procedures performed. Usually a patient can return to work in 2 to 4 weeks if they are able to work while seated. If a persons job requires standing and walking, return to work may take several weeks when one is able to bear weight. Complete recovery may take six months to a full year.
Potential Complications
Complications can occur as with all surgeries, but are minimized by strictly following your surgeons post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.