Information for WA Patients on Common Foot and Ankle Issues | Issaquah Foot & Ankle Specialists
-
Bone Bruise This is usually some type of impact injury to a bone that causes internal damage to the bone. This could be from a bad fracture or sprain involving the foot or ankle.This is a type of problem that one would not see on typical radiographs but rather one would be able to diagnose with an MRI.After the bone bruise there can be damage to the internal structure of bone in a specific location. For example this could involve a circular area that is 5 mm in diameter.
Within this area the blood supply to the bone becomes damaged and the bone itself may become nonviable. On MRI the radiologist may describe this as a focal area of bone marrow edema.What can happen with a bone bruise. The problem is, that a bone bruise doesn't always heal with normal bone healing and it can become a long-term cystlike area within the bone where there is an absence of normal bone structure. If this is in the middle of the bone it is possible for this to cause some deep discomfort and/or pain.But it also can cause a problem at this area of bone is directly beside a joint. The problem in this case would be that thebone directly beside the joint usually is supportive to the cartilage. Without the structure of the bone to support the cartilage can become damaged and loose. The cartilage can tear and can develop a defect such as an osteochondral defect within the ankle. Typically these don't heal well.What can be done, a very proactive treatment would be to take bone healing supplements right after any type of severe foot or ankle injury even if there has not been an MRI and even if there is not fracture involvement. This is proactive to help support the best possible outcome in regard to bonehealing from any potential underlying bone bruise.In addition. There are instances where an MRI has been ordered and bone bruise is identified by the radiologist. In this case if it is severe enough there are instances where may be helpful to order a bone stimulation device. For example some use the technology of pulsed electronegative magnetic fields, or ultrasound technology and these are routinely used with spinal fusions and often use with foot and ankle surgery involving bone healing.If they're not caught early and not treated early which is often the case, as mentioned above bone bruises often lead to long-term cystic changes within the bone and potentially problems with a lack of structure for the adjacent articular cartilage.At our clinic, we recommend Ortho Pro bono Bone healing supplements. -
Blood Clots In The Legs - Phlebitis There are two sets of veins which carry blood from the feet back to the heart and lungs. The superficial veins are located just beneath the skin, and are often visible as enlarged or varicose veins. The second network of veins are the deep veins which are located close to the bone of the leg and thigh, and are not visible. Each of these sets of veins has the potential to develop a blood clot.
A blood clot is referred to as a thrombosis. When a blood clot forms there is usually an inflammatory reaction. An inflamed vein is called phlebitis. The inflammation causes swelling, pain, redness, and warmth along the course of the vein. Because these two events (blood clot and inflammation) almost always occur together, the terms venous thrombosis and thrombophlebitis are both used to refer to a blood clot in a vein.
Under normal circumstances blood does not form a clot in the vein. There are certain things, which will make a clot more likely to occur. For example, some families have an unusual trait, which causes their blood to clot more than normal. This is a hereditary abnormality. More common causes of blood clots would include a direct injury to the vein, oral birth control pills, long hours of sitting (for example truck drivers), a recent surgery, prolonged periods of bed rest, a recent pregnancy, or the presence of some types of cancers. Each individual with a blood clot should be evaluated for the underlying cause.
Superficial Phlebitis
Diagnosis
When a thrombosis (blood clot) forms in a superficial vein in the foot or leg it is recognizable as a linear, firm cord. That is because these veins are inflamed and swollen, and because they are located just beneath the skin. They may appear red and feel warm from the inflammation. They are usually painful and very tender to pressure. Classically in the legs, these occur along the course of the greater or lesser saphenous veins. A blood test to evaluate white blood cells may be necessary to differentiate superficial phlebitis from cellulitus (an infection under the skin which can also lead to pain, swelling, and redness of the foot or leg).
Treatment
Superficial phlebitis, although painful, is not a serious condition. This condition should be evaluated by your doctor to rule out other more serious problems. Treatment usually involves the use of anti-inflammatory medication, elevation of the foot and leg, and warm compresses applied over the area of inflammation. Diabetic patients should not use heating pads or warm compresses unless they are supervised by their treating doctor.
Deep Vein Thrombosis
Diagnosis
Although occasionally asympotomatic, most people with deep vein clots complain of pain, swelling, and warmth of the leg. There may be swollen superficial veins as well. The leg pain and soreness is worse with standing or walking, and feels better with rest and elevation. When the area is examined there is often severe tenderness with deep pressure, although this could also be found with muscular problems in the same location.
Confirmation of a suspected deep vein thrombosis can be made by ultrasound testing or by venogram. These tests are important because it is sometimes difficult to establish the diagnosis without them. A proper diagnosis is essential with deep vein clots because failure to properly treat these can result in chronic venous insufficiency or a life threatening pulmonary embolus.
Treatment
Most patients with deep vein thrombosis require hospitalization. In this setting the patient will be given a blood thinner to prevent blood clots from spreading in the leg veins, and to prevent pieces of the clot (emboli) from traveling up to the lungs. Traditionally, heparin has been the blood thinner used in this situation. Other clot dissolving medications are now sometimes added to this treatment to prevent long term damage to the veins, thereby helping to preventing chronic venous insufficiency. Care must be taken with all these medication because they can result in serious undesirable bleeding. An additional treatment, which may be recommended, is a filter, which is surgically placed into the large vein returning blood to the heart. This filter is to prevent pieces of clots from traveling from the leg veins up to the heart and lungs. Clots in the lungs can cause death.
Once the patient has been stabilized, the heparin is discontinued and an oral blood thinner called warfarin (Coumadin) is used. This is usually continued for several months depending upon the severity of the episode, and the patient. Periodic blood tests are required to monitor the bleeding and clotting ability of the patient. The dose of the Coumadin is then adjusted as necessary.
Following an episode of deep vein thrombosis it is wise to wear a firm below knee elastic stocking (30 - 40 mm compression) to control swelling. Failure to wear an elastic stocking can lead to chronic venous insufficiency and it's associated problems including pain, swelling, dermatitis, skin discoloration, and ulcerations.
-
Blisters, Abrasions, And Skin Tears Blisters
 Blisters form as a result of heat, moisture and friction. Blisters can also form as a result of fungal infections of the skin, allergic reactions or burns. If a patient has diabetes, they should be evaluated by a doctor in a timely fashion. Generally, a person will recognize a burn by association with a specific painful event. People with diabetes may not be able recognize the painful event due to a condition called neuropathy. A doctor should attend to burns. Blisters are due to fungal infection of the skin or to allergic reactions, which will generally occur in clusters and be smaller than blisters caused by friction. They will also often occur in areas of the foot, which are free from friction forces.
Blisters form as a result of heat, moisture and friction. Blisters can also form as a result of fungal infections of the skin, allergic reactions or burns. If a patient has diabetes, they should be evaluated by a doctor in a timely fashion. Generally, a person will recognize a burn by association with a specific painful event. People with diabetes may not be able recognize the painful event due to a condition called neuropathy. A doctor should attend to burns. Blisters are due to fungal infection of the skin or to allergic reactions, which will generally occur in clusters and be smaller than blisters caused by friction. They will also often occur in areas of the foot, which are free from friction forces. Blisters should be drained leaving the cover of the blister in tact. The area should be protected with a non-stick bandage with mild compression. Ice to "hot spots" can be soothing and reduce the thermal damage to the surrounding area. "Double socking" can prevent blisters associated with athletics. Wearing two pair of socks allows the friction to be absorbed between the socks reducing friction to the skin. A sock has been developed that helps to reduce friction and blistering called the Thro-lo sock. It is useful for athletics and for diabetic patients. They are widely available in athletic shoe and apparel stores. Skin protectant sprays and adhesive gel pads are also available.
Blisters should be drained leaving the cover of the blister in tact. The area should be protected with a non-stick bandage with mild compression. Ice to "hot spots" can be soothing and reduce the thermal damage to the surrounding area. "Double socking" can prevent blisters associated with athletics. Wearing two pair of socks allows the friction to be absorbed between the socks reducing friction to the skin. A sock has been developed that helps to reduce friction and blistering called the Thro-lo sock. It is useful for athletics and for diabetic patients. They are widely available in athletic shoe and apparel stores. Skin protectant sprays and adhesive gel pads are also available.Abrasions
Abrasions to the skin are a result of excessive friction resulting in the partial loss of the epidermis. The area should be cleaned with an antibacterial soap and dressed with a non-stick bandage and a topical antibiotic ointment. It may take several weeks for the area to completely heal. During this period, the area should be protected from shearing forces. Deep abrasions can result in scaring. Any sign of infection should prompt a visit to the doctor.
Skin Tears
Skin Tears result from a rapid, forceful shear to the skin. Skin tears are most commonly self inflicted by improperly removing adhesive dressings and tape. Careful counter pressure should be applied to the skin near the adhesive dressing as the dressing or tape is slowly removed. A common misconception is that paper tape will not damage the skin. To the contrary this tape can really stick to the skin and will tear the skin if removed improperly.
-
Black Toenails Athletes will often encounter a problem with their toenails turning dark. This may be due to the toes hitting the end or the top of the shoe toe area. Quite often the toenail may become loose and fall off. This can also occur in people who have worn a tight shoe for a prolonged period of time. The dark color is a result of bruising under the toenail. Generally it is not painful. The damage caused to the toenail may allow the establishment of a fungal infection in the nail. In people who have diabetes, any change in the color of the toenail should be evaluated by a doctor. The pressure, which caused the bruising of the nail, can cause a small sore under the toenail, which can become infected.
Treatment
Treatment might consist of trimming the loose nail back and applying a topical anti-fungal medication. If the skin under the nail is ulcerated, then a topical antibiotic ointment should be applied. Patients with diabetes should not treat this condition themselves and should seek the advice of a doctor.
Prevention consists of wearing properly fitting shoes and possibly stretching of the calf muscles. People who are involved in athletics and exercise often have excessively tight calf muscles. This results in the muscles in the front of the leg having to work harder to pull the foot upward. This forces the toes to impact the top of the toe with greater force, potentially causing the bruising of the toenail.
-
Athlete's Foot (Tinea Pedis)  Athlete's foot is caused by a fungal infection of the skin on the foot. The majority of these infections are caused by one of three fungal agents called dermatophytes. Athlete's foot is by far the most common fungal infection of the skin. The infection can be either acute or chronic. The recurrent form of the disease is often associated with fungal-infected toenails. The acute form of the infection most often presents with moist, scaling between the toes with occasional small blisters and/or fissures. As the blistering breaks, the infection spreads and can involve large areas of the skin on the foot. The burning and itching that accompany the blisters may cause great discomfort that can be relieved by opening and draining the blisters or applying cool water compresses. The infection can also occur as isolated circular lesions on the bottom or top of the foot. As the skin breaks down from the fungal infection, a secondary bacterial infection can ensue.
Athlete's foot is caused by a fungal infection of the skin on the foot. The majority of these infections are caused by one of three fungal agents called dermatophytes. Athlete's foot is by far the most common fungal infection of the skin. The infection can be either acute or chronic. The recurrent form of the disease is often associated with fungal-infected toenails. The acute form of the infection most often presents with moist, scaling between the toes with occasional small blisters and/or fissures. As the blistering breaks, the infection spreads and can involve large areas of the skin on the foot. The burning and itching that accompany the blisters may cause great discomfort that can be relieved by opening and draining the blisters or applying cool water compresses. The infection can also occur as isolated circular lesions on the bottom or top of the foot. As the skin breaks down from the fungal infection, a secondary bacterial infection can ensue.Diagnosis
 The diagnosis of tenia pedis is generally made based upon the clinical presentation. A definitive diagnosis is made by taking a scraping of the skin and culturing it. It may take up to three weeks for the culture to grow the fungus. In some instances the culture may present a false negative result because the skin scraping was inadequate. Some doctors may perform a KOH prep of a skin scraping. This is examined under a microscope and may reveal elements that can make the diagnosis.
The diagnosis of tenia pedis is generally made based upon the clinical presentation. A definitive diagnosis is made by taking a scraping of the skin and culturing it. It may take up to three weeks for the culture to grow the fungus. In some instances the culture may present a false negative result because the skin scraping was inadequate. Some doctors may perform a KOH prep of a skin scraping. This is examined under a microscope and may reveal elements that can make the diagnosis.Athlete's Foot Treatment
Treatment should be directed at controlling the fungal infection and treating any secondary bacterial infection with oral antibiotics. Soaking the feet in Epsom salts and warm water is helpful. Wearing sandals to reduce moisture accumulation and heat generated by closed shoes will also help in the control and spread of the infection. Other conditions that mimic acute athlete's foot are contact dermatitis and pustular psoriasis.
The chronic form of athletes foot is a relatively noninflamatory type of infection. It is characterized by a dull redness to the skin and pronounced scaling. It may involve the entire bottom of the foot giving a "moccasin" appearance. It generally does not itch or result in the formation of blisters. This form of the disease frequently has an associated fungal infection of the toenails. There are good topical and oral medications available for the treatment of this condition. There are some less common causes of dry scaling skin on the feet.
-
Arthroscopy Of The Ankle And Subtalar Joints Arthroscopy is a surgical technique that involves the introduction of a small circular lens (2.0 to 6.0 mm in diameter) into a joint for the purpose of inspection and possible treatment. The arthroscope is an elongated tube possessing a series of lenses that allow for the magnification of structures within the joint. A camera is affixed to end of the arthroscope so that joint images can be projected onto a television monitor. Small incisions (one-quarter inch or less) are placed strategically around the joint to allow for the introduction of the arthroscope, as well as other pieces of equipment needed for the precise correction of joint injury.
Arthoscopy vs. Arthrotomy (Open Technique)
Arthroscopy offers several advantages over classical "open joint" (arthrotomy) techniques. First, arthroscopic evaluation and treatment only requires small incisions in the joint capsule, limiting the degree of scarring and trauma associated with surgery. Second, the environment within the joint is more easily inspected by virtue of the magnification provided by the arthroscope. Third, removal of damaged joint tissue or scarring is achieved in a more precise manner as a consequence of the very fine, specially designed equipment. Fourth, the joint is continuously bathed in physiological fluids providing a healthier environment during surgery. This is in contrast to open joint techniques where the cartilage surface is exposed to air within the operating room, potentially compromising its viability. Unfortunately, situations do arise when the joint needs to be opened in order to achieve the objectives of the surgical procedure. For example, certain cartilage injuries within the ankle joint may be located in areas where arthroscopic visualization is poor, or access to the lesion with available equipment is nearly impossible. In these cases, even though an arthrotomy was necessary due to inaccessibility, the arthroscope is invaluable in specifically identifying the location, and extent of the problem.
Ankle and Subtalar Anatomy
The ankle joint is comprised of three bones, the tibia (inner ankle and leg bone), the fibula(outer ankle and leg bone), and the talus (odd shaped, lower ankle bone). The ankle joint space is found between the talus and the tibia, as well as between the talus and the fibula. A large majority of the articular surface of the talus is in contact with the cartilage surface of the tibia. These two surfaces are slightly dome shaped from front to back. The ankle joint allows the foot to mobilize up (dorsiflexion) and down (plantarflexion). There are three major ligaments associated with the outer part of the ankle joint: the Anterior Talofibular, Calcaneofibular, and Posterior Talofibular ligaments. There is one major ligament with several bands associated with the inner part of the joint: the Deltoid ligament. Together these ligaments guide motion and provide stability to the ankle joint.
The lower ankle joint or subtalar joint (below the talus) exists between the talus and the heel bone (calcaneus). The subtalar joint is actually made up of two anatomically distinct joints. These two joints are separated by a void or space, which houses the two major ligamentous stabilizers of the subtalar joint: the Interosseous Talocalcaneal and Cervical Ligaments. Further stability is afforded to the subtalar joint by one of the three lateral ankle ligaments (Calcaneofibular Ligament), and several bands of the main inner or medial ankle ligament (Deltoid Ligament). The subtalar joint allows the foot to pronate and supinate. Supination of the subtalar joint involves movement of the foot in an inward direction, so that the sole of the foot faces the opposite limb. Pronation of the subtalar joint involves movement of the foot in an outward direction, allowing the sole to face away from the opposite limb.
Rearfoot and Ankle Inversion Injuries: Mechanism of Injury
During a common ankle sprain, the foot is forcibly rotated inward toward the opposite leg. The inward movement of the foot is a motion well accommodated by the lower ankle joint (subtalar joint), but not by the upper or true ankle joint. Ultimately, the lower ankle joint comes to the end of its available inward motion, and stops rather abruptly (the lower ankle joint can be injured at this point). Continued inward movement of the foot forces the ankle joint in a direction it is not designed to accommodate. The lower ankle bone or talus is thus forcibly directed inward, partially dislocating the talus out from under the tibia and fibula. It is not uncommon for the outer ankle ligaments to be partially or completely torn, resulting in joint instability. Furthermore, the adjacent joint surfaces can collide or impinge during the injury, resulting in disruption of the cartilage surface.
Arthroscopy: Indications for usage
Arthroscopy is an effective tool for the evaluation and management of pain localized to the ankle or lower ankle (subtalar) joints. Following an ankle sprain, ligamentous scarring can occur within various regions of the ankle or subtalar joints. Arthroscopy allows direct visualization and precise removal of scar tissue with minimal joint trauma. Generally, two to four portals or incisions are required for ankle arthroscopy, and two or three for subtalar arthroscopy. Loose fragments of bone, cartilage or ligament can be identified and removed through the small portals in the joint capsule. Occasionally, small accessory incisions may be necessary to remove larger fragments of tissue found within the joint. Regions of the joint surface that have been injured will commonly display an obvious defect or a loose flap of cartilage that has been delaminated from the underlying bone. Not infrequently, the joint surface will appear normal; however, gentle probing will reveal an area of softness compared to surrounding cartilage. These soft areas are regions of cartilage injury and will require removal of the damaged cartilage. In some cases, physicians are drilling small holes through these soft zones in order to promote re-adhesion of the cartilage. In areas where there is an obvious defect in the cartilage surface, the damaged cartilage is removed down to normal cartilage. Following the removal of damaged cartilage, the exposed underlying bone is drilled repetitively to facilitate bleeding into the base of the injured area. The blood will form a clot across the full dimensions of the defect. Over time the blood clot is converted to cartilage. The repair cartilage is not of the same quality as was originally present; however, the repair cartilage re-establishes near normal surface-to-surface contact. In some cases, small plugs of normal cartilage and bone can be removed from one location within the ankle joint, and placed into an area of cartilage injury. Unfortunately, transport of cartilage within the ankle joint necessitates an open joint technique and cannot be performed arthroscopically.Arthroscopy has also been useful in assisting with the repair of fractures that involve the surfaces of the ankle joint (Pilon fractures or talar fractures). In these cases, the arthroscope is used to visualize the fractured joint surface as it is repaired to assure accurate realignment. Arthroscopy has also been used to visualize the joint during removal of the articular cartilage prior to fusion of the ankle joint.
Conditions Where Arthroscopy may not be Useful
Unfortunately, arthroscopy is not helpful in certain types of joint injury. If a cartilage lesion is located in the central or back portion of the joint, many times the lesion cannot be accessed with the arthroscope. In these cases, the tibia or inner ankle bone must be cut in order to allow inspection and treatment of the lesion. Ankle fusions cannot be performed arthroscopically if a large degree of malalignment exists within the ankle joint itself. In these cases, the joint must be opened and the joint surface remodeled to reduce the deformity. Although some surgeons are repairing single ligament tears through the arthroscope, this has not gained universal acceptance. Significant joint instability associated with multi-ligament injury requires open joint repair or reconstruction techniques.
Arthroscopic Surgery of the Ankle and Subtalar Joints
Arthroscopic surgery of either the ankle or subtalar joints is generally considered an outpatient (same day) surgical procedure. Pre-operatively or intra-operatively, patients are usually given antibiotics to reduce the risk of infection. The surgery can be performed under either general or spinal anesthesia. Arthroscopy can also be performed under local anesthesia with IV sedation. The latter procedure requires the anesthesiologist to use a local anesthetic to block the large nerve behind the knee joint (main nerve block). The surgeon will further supplement the main block with local anesthetic infiltrated just above the ankle joint. The patient is then kept in a twilight sleep with medications infiltrated through the IV by the anesthesiologist. Post-operatively, the ankle is lightly bandaged. The patient may be placed in a removable cast boot or splint to keep the ankle at 90 degrees to the leg; however, gentle range of motion is recommended on a regular basis after surgery. Following surgery, patients are usually non-weight bearing for 7-14 days, and then are allowed to weight bear as tolerated. If a large cartilage lesion was either drilled or cleaned out, patients will remain non-weight bearing up to 4 weeks. The actual duration of non-weight bearing will depend on the extent of the injury and the type of treatment rendered. It is not uncommon for patients to undergo physical therapy after surgery, especially if they had a prolonged period of pain and disuse prior to surgery.
Risks and Complications Associated with Ankle or Subtalar Arthroscopy
Like any other surgical procedure, arthroscopy has certain inherent risks and complications. In the author's experience, these have been uncommon. The literature sites injuries to the superficial nerves as the most common complication after ankle arthroscopy. Most of these nerve related injuries result in tingling, numbness, or occasionally burning sensations across the outer part of the ankle onto the top of the foot. Most of these sensations resolve over a period of 3-5 months. Obviously, more significant nerve related injuries have been reported, but they are uncommon. There is the risk of infection; this complication is rarely seen with appropriate antibiotic prophylaxis prior to surgery and sterile technique during surgery
Conclusions
Arthroscopy of the ankle or subtalar joints has proven to be a valuable tool for treating various injuries to these unique joints. The degree of joint and soft tissue trauma associated with arthroscopy is no doubt less than open joint techniques, resulting in somewhat faster healing times. Immediate return to walking and sports is not usually recommended. The joint can be often sore and swollen for several weeks after surgery. Aggressive and rapid return to activity can result in a more prolonged recovery time. Listen to physician instructions and follow carefully.
-
Arthritis Of The Big Toe Joint Stiffness of the big toe joint is termed Hallux Limitus. Hallux is the medical term for the big toe. When the big toe possesses no motion, it is termed Hallux Rigidus. To confuse the topic, the big toe joint may appear to have normal motion, but this motion can be limited when weight is on the foot and during the normal standing and walking. This is termed functional Hallux limitus, because it occurs during the normal functioning of the foot while walking. As with many conditions that affect the foot, functional conditions progress to structural deformities. As the condition progresses, a degenerative type of arthritis develops in the big toe joint.
Diagnosis
The most common cause of Hallux limitus is an abnormal alignment of the long bone behind the big toe joint called the first metatarsal bone. In this condition, the first metatarsal bone is elevated relative to the other metatarsal bones that lie behind the other toes. When this is the case, the big toe joint cannot move smoothly and jamming occurs at the joint. A variety of symptoms can begin to occur. One common problem that occurs is pain in the bottom of the big toe where a central callus can develop. The pain and callus develop because the big toe does not bend upward enough as the bottom of the toe is jammed into the ground. People who have diabetes must watch this area carefully because the pressure can cause the development of an ulceration that can become infected.
Another consequence of the jamming of the big toe joint is the development of bone spurs on the top of the joint. This bump on the top of the big toe joint can become painful as a result of shoe pressure. Pain within the joint is a common result of the limitation of movement of the big toe joint. With time, the big toe joint becomes stiff and painful to move. As the joint continues to degenerate more bone spurring occurs. If the condition is left untreated complete destruction of the joint can occur.
Diagnosis is made by performing a physical exam of the foot and the use of x-rays. In early stages of the condition x-rays may be normal. In later stages of the condition, narrowing of the joint and/or bone spurs may be evident.
Treatment
Initial treatment consists of using oral anti-inflammatory medications, cortisone injections and/or functional orthotics. Oral medications and cortisone injections are useful in treating the pain associated with the condition, but will not stop the process because they do not address the underlying cause of the condition. Functional orthotics, however, are designed to treat the cause of the condition. These devices will generally fit into normal shoes and correct the underlying functional problem with the joint. Orthotics will not reverse what damage may have occurred, but can slow or halt the on-going damage to the joint.
If the condition progresses to the point of spurring around the joint, surgery may be indicated. Depending upon the degree of degeneration of the joint, surgery may consist of simply removing the bone spurs around the joint, a decompresion osteotomy or may require a total joint replacement or joint fusion. Following surgery, the use of a functional orthotic is useful to improve the joint function.
If a painful callous exits on the bottom of the big toe it will frequently resolve and the pain subside with the use of functional orthotics and/or surgery to improve the motion of the joint.
-
Ankle Sprains Ankle sprains are very common and happen when an unnatural movement (such as a roll, twist or turn) occurs, which can stretch or tear the ligaments that help hold the ankle together.
You should always seek medical attention with a sprained ankle so the severity of the sprain can be assessed and a proper treatment plan can be put in place.
Something that our doctors will recommend to many of their ankle sprain patients is at-home exercises, which will help speed up the recovery process and re-build the strength needed in the ankle. There are three main reasons why exercises are crucial for patients to perform:
- It's imperative to restore to normal what's known as "range of motion"
- Strength must be rebuilt so a repeat injury isn't more likely to occur
- The nerves, muscles and ligaments in the ankle need to be retrained to respond to the body's different movements
Often some gentle range of motion exercises are recommended. These can include "writing" the alphabet with the big toe. An active ankle brace or other ankle brace while doing this exercise may help reduce swelling and pain. Keeping an ice pack on the ankle while doing this exercise is also helpful.
After a few days of "writing" the alphabet, you may be able to move on to other stretches, such as the towel stretch. Fold a towel lengthwise and position it around your forefoot. Gently flex your foot upward. These types of exercises should only be performed if directed by a doctor to do so. Otherwise more damage to the ankle may occur if the sprained ankle is misdiagnosed.
Please keep in mind that before starting these exercises, you need to be evaluated by a doctor to determine if these exercises are right for you.
Ankle sprains are one of the most common injuries we see at Issaquah Foot & Ankle Specialists. They are also one of the most under treated injuries in medicine. Patients often do not seek treatment or do not follow up after the initial visit which often takes place in the emergency room. This can have devastating consequences for the long term function of the ankle. Ankle sprains can injury the following structures:
- Ligaments
- Tendons
- Cartilage
- Bone
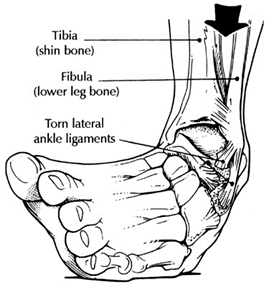
The above picture demonstrates the lateral ligament complex of the ankle. You can see the anterior talofibular ligament which is the most common ligament injured following an ankle sprain. The calcaneofibular can be injured as well, however this is less common. Ligaments can take 6-8 weeks to completely heal if a tear does occur. It is essential to seek medical treatment from a foot and ankle specialist. They will guide you in rehabilitation to allow adequate time for ligaments to heal and appropriate strengthening exercise to speed recovery.
Repeated ankle injury can lead to Chronic Ankle Instability or Chronic Ankle Sprains
 Chronic ankle instability is the recurring “rolling” or “giving away” of the outer side of the ankle. The ligaments on the lateral side of the ankle may become weakened over time and after repeated ankle sprains. Typically the “rolling” or “giving away” occurs when walking or being active. This is a common occurrence with athletes. However, this can even happen when simply standing.
Chronic ankle instability is the recurring “rolling” or “giving away” of the outer side of the ankle. The ligaments on the lateral side of the ankle may become weakened over time and after repeated ankle sprains. Typically the “rolling” or “giving away” occurs when walking or being active. This is a common occurrence with athletes. However, this can even happen when simply standing.Symptoms:
Symptoms of chronic ankle instability may include pain, swelling or tenderness of the area. The most obvious symptom is the frequent rolling or turning of the ankle.
Causes:
Chronic ankle instability is generally caused by an ankle sprain that has not healed completely. When the ankle is sprained the ligaments are damaged. These ligaments, depending on the severity of the injury, are either stretched or torn. The image on the top right shows these ligaments as being wavy. This is how the ligaments appear after being stretched as a result of an ankle sprain. These stretched ligaments can lead to chronic ankle instability if they are not properly healed.
Diagnosis:
If you experience frequent ankle sprains or chronic instability in your ankles you should have this evaluated by us. If this condition is left untreated it can lead to further complications. The instability can lead to injuries as a result of a fall and arthritis and tendon problems. Depending on your circumstances an x-ray, CT scan, or MRI may be ordered to determine the best course of action.
Treatment:
Based on the examination results surgery may or may not be necessary. Nonsurgical treatments include physical therapy to rehabilitate and strengthen the muscles. Bracing can be effective by offering support to the ankle and prevent abnormal movement. Nonsteroidal anti-inflammatory drugs like ibuprofen can reduce swelling and pain. If the problem is severe surgery may be necessary. If the instability is significant and non-surgical methods do correct the issue reconstructive surgery to repair the ligaments will correct this issue.
Other common causes of ankle pain
There are many reasons for ankle pain; some of the most common include a history of ankle sprains or trauma. Trauma or sprains can often result in inflammation of the ankle joint or damage to soft tissue structures like ankle ligaments or tendons. The anterior talar fibular ligament or peroneal tendons are often injured with sprains.
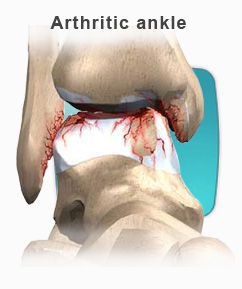
Patients often relate a stiffness, popping or catching of the ankle as part of these symptoms. These can be attributed to other causes including arthritis of the ankle or damage to cartilaginous surfaces.
There are a variety of treatment options from conservation care to surgical reconstruction.
-
Foot and Ankle pain Quite a few patients, especially runners or athletes come in with:
- ankle and foot pain
- ankle and foot pain after running
- ankle and foot pain without swelling
There are many reasons for ankle pain, some of the most common include a history of ankle sprains or trauma. Trauma or sprains can often result in inflammation of the ankle joint or damage to soft tissue structures like ankle ligaments or tendons. The anterior talar fibular ligament or peroneal tendons are often injured with sprains.
Patiens often relate a stiffness, popping or catching of the ankle as part of there symptoms. These can be attributed to other causes including arthritis of the ankle or damage to cartilaginous surfaces.
There are a variety of treatment options from conservation care to surgical reconstruction.
Common Foot And Ankle Disorders
Did you know the foot has 26 bones, 33 joints, 107 ligaments, 19 muscles, and numerous tendons? These parts all work together to allow the foot to move in a variety of ways while balancing your weight and propelling you forward or backward on even or uneven surfaces. It is no wonder that 75 percent of all Americans will experience foot problems at one point or another in their lifetimes. At Issaquah Foot and Ankle Specialists we know what you're looking for in a foot doctor and we know we have the best foot care in the Seattle area. Our office can help diagnosis and treat your foot and ankle disorders from Flatfoot to Foot Reflexology, we consider all cases and all methods of pain relief. Click on the categories below to read articles on foot disorders and conditions.
Pain Experienced by the Walking Child
-
Peroneal Tendon Dysfunction Dislocating peroneal tendons are an uncommon injury to a group of two tendons whose muscles originate on the outside of the calves. These two muscles are named the Peroneus Brevis and Peroneus Longus. These two muscles are responsible for eversion of the foot. This movement of the foot is demonstrated by standing and then rolling to the outside of the foot. These tendons are also called "stirrup" tendons because as they pass into the foot they act as a stirrup to help hold up the arch of the foot. As these tendons pass behind the outside ankle bone, called the fibula, they are held in place by a band of tissue called the peroneal retinaculum. Injury to the retinaculum can cause it to stretch or even tear. When this occurs the peroneal tendons can dislocate from their groove on the back of the fibula. The tendons can be seen to roll over the outside of the fibula. This will cause the tendons to function abnormally and can cause damage to the tendons. Dislocating peroneal tendons most commonly occur as a result of injury during participation in athletic activities. The most common sport causing injury is snow skiing. It can also occur while playing football, basketball, and soccer. This injury can occur in non-athletes, as a result of a severe ankle sprain. The injury typically results in a popping or sharp pain on the outside of the ankle. The outside of the ankle is called the lateral malleolus. Commonly however, there may be little to no discomfort at the time of injury, which later becomes symptomatic. Diagnosis
Physical examination will reveal swelling behind the outside of the ankle if it is an acute injury. If the injury is chronic there may be little to no swelling. There is usually tenderness particularly when pressure is applied behind the outside of the ankle. Having the patient forcefully turn the foot outward against the physician's hand can demonstrate dislocation of the peroneal tendons. This will cause the peroneal tendons to dislocate over the outer edge of the lateral malleolus.
X-rays and occasionally an MRI exam may be necessary to confirm the diagnosis. X-rays are commonly taken to ensure that there are not any other injuries to the bones of the foot and ankle. An MRI will provide your physician with information about abnormal positioning and/or possible tears of the peroneal tendons.
Treatment
Non Surgical Treatment
If there is an acute injury the initial treatment is usually crutches with no weight being applied to the foot. Usually a splint or compressive wrap is applied to decrease swelling. Anti-inflammatory medications and ice are often utilized to help decrease swelling. Once the swelling has subsided your physician will be better able to tell the true extent of injury. Mild injury can be treated with conservative, non-surgical means. Mild injury results in stretching of the peroneal retinaculum without dislocation of the peroneal tendons. The patient is placed in a cast or removable cast boot and must use crutches for six weeks. During this time no weight can be applied to the foot. After six weeks the patient is re-examined. If the injury has not healed further treatment may be necessary.
Surgical Treatment
Surgical correction is necessary in cases of failed conservative therapy and moderate to severe injuries. With moderate to severe injuries the peroneal retinaculum is either torn or severely stretched to a point that the peroneal tendons will easily dislocate. Surgery will involve tightening the stretched or torn peroneal retinaculum. Both absorbable and non-absorbable suture or stitches will be necessary to hold the tissue in place until it heals. This may require drill holes or metallic anchors to be placed in the fibula to aid in suturing the peroneal retinaculum back onto itself.Twenty-five percent of the population does not have a groove on the back of the fibula for the peroneal tendons to move in. This groove is called the peroneal groove. This can be a causative factor for peroneal tendon dislocation and can only be identified at the time of surgery. If this is encountered during surgery a peroneal groove will be created by performing bone cuts in the back of the fibula. These may require bone screws or pins to hold the bone in place while it heals. During the surgery the peroneal tendons will be examined for possible tears or damage. If this is found it will be repaired by suture.
Post-operatively the patient is placed on crutches and in a splint or cast for 4 to 6 weeks with no weight being applied to the foot. This is followed by 2 to 4 weeks of protected weight bearing in a cast or removable cast boot. This is usually followed by 3 to 6 weeks of physical therapy to regain strength and motion.
Potential Complications
Once an injury occurs it is always possible for a person to re-injure or re-dislocate their peroneal tendons. Surgical complications are rare but can include: infection, reoccurrence, stiffness and weakness of the peroneal tendons, and delay or failure of bone cuts in the fibula to heal. The risk for complications is greatly reduced by taking your prescriptions as instructed and strictly following post-operative instructions.
Page 14 of 21







