What is Equinus?
Equinus is a condition in which the upward bending motion of the ankle joint is limited. Someone with equinus lacks the flexibility to bring the top of the foot toward the front of the leg. Equinus can occur in one or both feet. When it involves both feet, the limitation of motion is sometimes worse in one foot than in the other.
 People with equinus develop ways to "compensate" for their limited ankle motion, and this often leads to other foot, leg, or back problems. The most common methods of compensation are flattening of the arch or picking up the heel early when walking, placing increased pressure on the ball of the foot. Other patients compensate by "toe walking," while a smaller number take steps by bending abnormally at the hip or knee.
People with equinus develop ways to "compensate" for their limited ankle motion, and this often leads to other foot, leg, or back problems. The most common methods of compensation are flattening of the arch or picking up the heel early when walking, placing increased pressure on the ball of the foot. Other patients compensate by "toe walking," while a smaller number take steps by bending abnormally at the hip or knee.
Causes
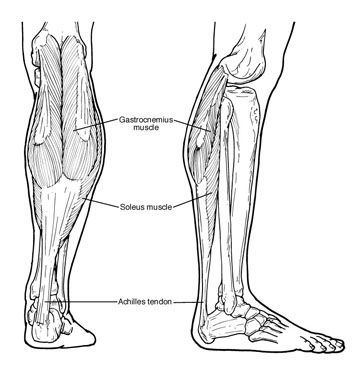
There are several possible causes for the limited range of ankle motion. Often it is due to tightness in the Achilles tendon or calf muscles (the soleus muscle and/or gastrocnemius muscle). In some patients, this tightness is congenital (present at birth) and sometimes it is an inherited trait. Other patients acquire the tightness from being in a cast, being on crutches, or frequently wearing high-heeled shoes. In addition, diabetes can affect the fibers of the Achilles tendon and cause tightness.
Sometimes equinus is related to a bone blocking the ankle motion. For example, a fragment of a broken bone following an ankle injury, or bone block, can get in the way and restrict motion.
Equinus may also result from one leg being shorter than the other.
Less often, equinus is caused by spasms in the calf muscle. These spasms may be signs of an underlying neurologic disorder.
Foot Problems Related to Equinus
Depending on how a patient compensates for the inability to bend properly at the ankle, a variety of foot conditions can develop, including:
- Plantar fasciitis (arch/heel pain)
- Calf cramping
- Tendonitis (inflammation in the Achilles tendon)
- Metatarsalgia (pain and/or callusing on the ball of the foot)
- Flatfoot
- Arthritis of the midfoot (middle area of the foot)
- Pressure sores on the ball of the foot or the arch
- Bunions and hammertoes
- Ankle pain
- Shin splints
Diagnosis
Most patients with equinus are unaware they have this condition when they first visit the doctor. Instead, they come to the doctor seeking relief for foot problems associated with equinus.
To diagnose equinus, the foot and ankle surgeon will evaluate the ankle's range of motion when the knee is flexed (bent) as well as extended (straightened). This enables the surgeon to identify whether the tendon or muscle is tight and to assess whether bone is interfering with ankle motion. X-rays may also be ordered. In some cases, the foot and ankle surgeon may refer the patient for neurologic evaluation.
Non-Surgical Treatment
Treatment includes strategies aimed at relieving the symptoms and conditions associated with equinus. In addition, the patient is treated for the equinus itself through one or more of the following options:
- Night splint. The foot may be placed in a splint at night to keep it in a position that helps reduce tightness of the calf muscle.
- Heel lifts. Placing heel lifts inside the shoes or wearing shoes with a moderate heel takes stress off the Achilles tendon when walking and may reduce symptoms.
- Arch supports or prescription custom orthotics devices. Prescription custom orthotics devices that fit into the shoe are often prescribed to keep weight distributed properly and to help control muscle/tendon imbalance.
- Physical therapy. To help remedy muscle tightness, exercises that stretch the calf muscle(s) are recommended.
When is Surgery Needed?
In some cases, surgery may be needed to correct the cause of equinus if it is related to a tight tendon or a bone blocking the ankle motion. The foot and ankle surgeon will determine the type of procedure that is best suited to the individual patient.






 Flatfoot is often a complex disorder, with diverse symptoms and varying degrees of deformity and disability. There are several types of flatfoot, all of which have one characteristic in common: partial or total collapse (loss) of the arch.
Flatfoot is often a complex disorder, with diverse symptoms and varying degrees of deformity and disability. There are several types of flatfoot, all of which have one characteristic in common: partial or total collapse (loss) of the arch.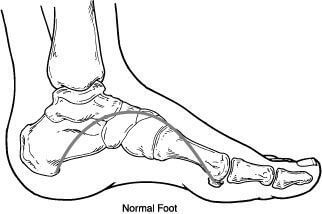 Flexible flatfoot is one of the most common types of flatfoot. It typically begins in childhood or adolescence and continues into adulthood. It usually occurs in both feet and progresses in severity throughout the adult years. As the deformity worsens, the soft tissues (tendons and ligaments) of the arch may stretch or tear and can become inflamed.
Flexible flatfoot is one of the most common types of flatfoot. It typically begins in childhood or adolescence and continues into adulthood. It usually occurs in both feet and progresses in severity throughout the adult years. As the deformity worsens, the soft tissues (tendons and ligaments) of the arch may stretch or tear and can become inflamed.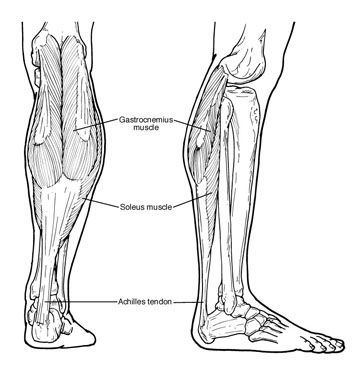 People with equinus develop ways to "compensate" for their limited ankle motion, and this often leads to other foot, leg, or back problems. The most common methods of compensation are flattening of the arch or picking up the heel early when walking, placing increased pressure on the ball of the foot. Other patients compensate by "toe walking," while a smaller number take steps by bending abnormally at the hip or knee.
People with equinus develop ways to "compensate" for their limited ankle motion, and this often leads to other foot, leg, or back problems. The most common methods of compensation are flattening of the arch or picking up the heel early when walking, placing increased pressure on the ball of the foot. Other patients compensate by "toe walking," while a smaller number take steps by bending abnormally at the hip or knee.
