In some foot and ankle conditions, your doctor may order an MRI to help diagnosis the problem that you are having with your foot and ankle. In the foot and ankle, MRI can be used to diagnosis the following conditions:
- Tendon injuries
- Ligament injuries
- Cartilage injuries
- Fractures
- Tumors (soft tissue and bone)
- Infection
- Avascular necrosis
- Non-unions or delayed unions of bone fractures
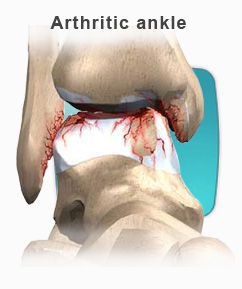
- Arthritis
What is MRI?
MRI is the newest way to view the human body since the CT (CAT) scanner was invented. Unlike CT scans, MRI does not use radiation in the conventional sense of the word. Rather, it combines the use of a large magnet and radio waves. The hydrogen atoms in the patient's body react to the magnetic field, and a computer analyzes the results and makes pictures of the inside of your body. MRI pictures show the soft tissues and bones of the foot and ankle in a cross sectional fashion. In many situations MRI offers unique information to help your doctor better plan your treatment and care.During the scan you will be lying inside a large tubular donut-shaped machine. Typically only your leg will go into the machine and the rest of your body will be outside of the tube. The radiographers want you to be comfortable and will ask you to be very still during the scan because even slight movement can spoil the images and reduce their usefulness to you and your doctor. Because the MRI uses a large magnet to create the images during the exam, you will hear a series of loud knocking sounds. You must remain very still at this time, as this is when the pictures are being taken. The inside of the scanner is well lit, and has a fan to blow fresh air gently over you. Music is typically provided if needed and the radiographers will talk to you through an intercom system to tell you want is going on.
Preparation for MRI
In most cases there is no special preparation for an MRI scan. You can eat and drink normally on the day of the scan although it is best to avoid large amounts of coffee or other things that make you restless. It is very important not to bring any metal into the scan room without letting the Radiographer know. Before the scan you will be asked to remove your watch, keys, coins, credit cards, bus tickets and phone cards. The strong magnet of the MRI scanner can damage all these, or they might cause distortions in the MRI pictures. When you arrive at MRI, you will be asked a series of questions to find out if you have any metal or implants in your body.
Getting Comfortable & Keeping Still
MRI images are very sensitive to movement. By keeping very still during the scan you can improve the quality of the images that are obtained. We have found that the best way to keep still is to be relaxed, lying comfortably as if you were dropping off to sleep. The MRI Radiographer is very interested in making you comfortable in the scanner so that you feel settled, secure and relaxed, let them know what they can do for you and together you will ensure the best possible pictures.
Problems with MRI
It may not be possible, or safe, to have a MRI scan if you have any of these items:
- Cardiac pacemaker
- Surgical clips in your head (particularly aneurysm clips)
- some artificial heart valves
- Electronic inner ear implants (bionic ears)
- Metal fragments in your eyes
- Electronic stimulators
- Implanted pumps
People with dental fillings and bridges, hip and knee replacements, and tubal ligation clips can all be scanned safely. The Radiographers will want to know about these things to minimize the effect they have on your images.
Claustrophobia
If you have experienced claustrophobia, or have trouble in enclosed spaces talk about it with the MRI staff before your appointment date. For mild claustrophobia, the staff can help you to relax enough to get rid of the anxiety in a few minutes. If your claustrophobia is severe you may need an anti-anxiety prescribed by your referring doctor. Staff at the MRI unit can be contacted about this and can offer your doctors some advice. You shouldn't drive after taking such drugs, so arrange a safe way to get home. Because there are no side effects of MRI you can bring a friend into the scan room for support if that will help your anxiety. Children in particular should feel free to bring an adult in with them. Everyone coming into the scan room will be asked the questions about metal and implants.
Contrast Injections (Dye)
Most MRI tests do not need you to have an injection, but in some situations a contrast agent can greatly improve the accuracy of the scan. The contrast is injected into a vein, and the dose is quite small. MRI contrast is not the same as X-ray contrast. Very few people notice when it is injected. Make sure to tell the technologist if you have any allergies to contrast dye.
Pregnancy
If you are pregnant or could be pregnant at the time of your scan appointment, please call us early so we can discuss the situation with you and consult your doctor. MRI causes a slight heating of your body, so most MRI sites avoid scanning during the first 3 months of pregnancy unless the diagnosis cannot wait and the only alternative test uses X-rays. Beyond that period, MRI is still avoided if the diagnosis can wait till your child is born as a matter of extreme caution. In many sites around the world MRI is used to examine pregnant women and their babies to avoid the need for X-ray tests. MRI contrast is not used during pregnancy.
How long does the MRI take?
Each test is specifically tailored to your needs. Several pictures may be needed to complete the exam. Each picture can take anywhere from a few seconds to fifteen minutes. A full exam of the foot and ankle could take anywhere from one hour to an hour and a half. The length of the exam depends on the area being tested and if any contrast is used.
Results
MRI scans are usually not reported while you are at the MRI Unit. The images are filmed by the Radiographer who scans you, and then later interpreted by a specialist called a Radiologist. Their report is sent with the MRI films and any private films you brought along, to the doctor who referred you. This delivery usually takes several days.





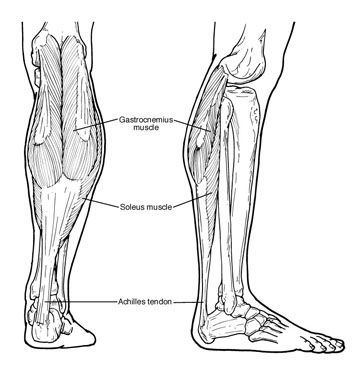 People with equinus develop ways to "compensate" for their limited ankle motion, and this often leads to other foot, leg, or back problems. The most common methods of compensation are flattening of the arch or picking up the heel early when walking, placing increased pressure on the ball of the foot. Other patients compensate by "toe walking," while a smaller number take steps by bending abnormally at the hip or knee.
People with equinus develop ways to "compensate" for their limited ankle motion, and this often leads to other foot, leg, or back problems. The most common methods of compensation are flattening of the arch or picking up the heel early when walking, placing increased pressure on the ball of the foot. Other patients compensate by "toe walking," while a smaller number take steps by bending abnormally at the hip or knee.
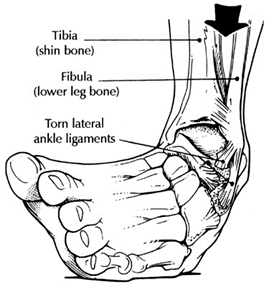 Chronic ankle instability is the recurring “rolling” or “giving away” of the outer side of the ankle. The ligaments on the lateral side of the ankle may become weakened over time and after repeated ankle sprains. Typically the “rolling” or “giving away” occurs when walking or being active. This is a common occurrence with athletes. However, this can even happen when simply standing.
Chronic ankle instability is the recurring “rolling” or “giving away” of the outer side of the ankle. The ligaments on the lateral side of the ankle may become weakened over time and after repeated ankle sprains. Typically the “rolling” or “giving away” occurs when walking or being active. This is a common occurrence with athletes. However, this can even happen when simply standing.