Plantar fasciitis typically causes pain in the bottom of the heel. People who have plantar fasciitis know how it classically hurts first thing in the morning and it hurts when they gets up from sitting, this is called post-static dyskinesia. Post-static dyskinesia can simply be referred to as pain after rest.
Many of the other causes of heel pain that are part of the differential diagnosis for plantar fasciitis, do not have this poststatic dyskinesia or first thing in the morning heel pain. With plantar fasciitis, limping in the morning is classic. At our clinic, we have seen patient's over the years that had these classic plantar fasciitis-like symptoms. However on further examination, they have a very thin plantar fat pad and with diagnostic imaging such as diagnostic ultrasound imaging the plantar fascia shows no inflammation or edema.
Some of these individuals also have a very high arch foot structure so that the contact points of the heel and the forefoot are more intense and focal than someone with a flatfoot or even a normal arch. With this problem, people are virtually walking on the heel bone. Some people are structurally born and develop this way. Other people have a normal healthy fat pad cushion, but over time the fat pad breaks down causing this problem. It is more common as one gets older. This is also called atrophy of the plantar fat pad or atrophic plantar fat pad.
How is this diagnosis made?
- A thin fat pad seen during physical exam or direct measurement.
- The exclusion of plantar fasciitis
- Often there is a higher arch foot structure
Usually there is immediate relief by wearing good shoes or a cushioning device. One can measure the thickness of the plantar fat pad with diagnostic ultrasound imaging, CT scan or an MRI.
Treatment for this is usually mechanical in nature. This includes not going barefoot and using specific shoes that have excellent cushioning such as some better running shoes. But also, some of the rocker shoes such as the MBT or Sketcher shape up shoes are very effective at shifting pressure off the heel. In addition to this, a gel heel cushion, or a heel cup can be helpful.
The most effective long-term treatment is an custom prescription orthotic with a very deep heel cup that actually has a hole in the bottom of the heel but is filled with 1/8 inch neoprene it is covered with a special cushioning material called poron and has a cushioned top cover on the entire orthotic including the deep heel cup area. This way, one is using the natural contour of the heel and the existing fat pad to help cushion the bottom weight-bearing portion of the heel bone. In chronic cases that do not fully respond to mechanical treatment including the special orthotics, and we will occasionally do a low dose ultrasound-guided cortisone injection. In this case the cortisone is injected directly at the layer between the plantar fascia and the fat pad. The goal is to avoid injecting into the fat pad. Repeated cortisone injections directly into the fat pad are thought to promote atrophy and further thinning of the fat pad.
If you experience this type of pain you can read more information about heel pain at our heel pain center on our website.


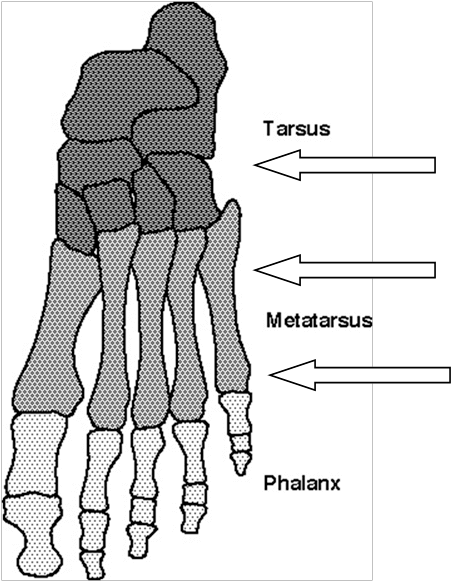
 The pediatric foot is a complex instrument that must be carefully evaluated.
The pediatric foot is a complex instrument that must be carefully evaluated.