Symptoms and Effective Treatment for Sever’s Disease
Sever's disease, also known as calcaneal apophysitis, is a common but often misunderstood condition affecting children and adolescents, especially those active in sports. It is not a traditional disease but rather a painful growth plate disorder. Understanding its symptoms and appropriate treatment is vital for parents and young athletes. The hallmark symptom of Sever's disease is heel pain, typically at the back or along the bottom of the heel. Pain tends to worsen during or after physical activities and may cause limping or discomfort when walking or running. The condition arises when the growth plate at the back of the heel bone becomes inflamed due to repetitive stress. Fortunately, Sever's disease is treatable. Getting adequate rest and taking over-the-counter pain relievers can help alleviate discomfort. Stretching exercises and may also be recommended to improve flexibility, and strengthen the calf muscles. Wearing supportive footwear with cushioned insoles may help reduce heel pressure. By recognizing the symptoms and seeking appropriate treatment, parents and young athletes can manage Sever's disease effectively, allowing for a smoother path to recovery and a return to their favorite activities. If your active child has heel pain, it is strongly suggested that you consult a podiatrist who can accurately diagnose and treat Sever’s disease.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see the podiatrists from Issaquah Foot & Ankle Specialists. Our doctors can treat your child’s foot and ankle needs.
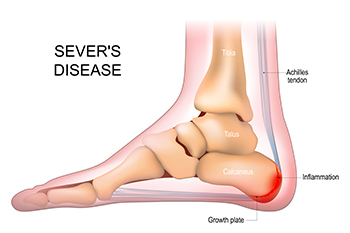
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact one of our offices located in Issaquah, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Sever's Disease
Sever’s disease, also known as calcaneal apophysitis is a common bone disorder that occurs during childhood. The disease is defined as an inflammation of the growth plate in the heel. When a child has a growth spurt, his heel bone grows faster than the muscles, tendons, and ligaments in his leg. This disease is a result of overuse. The people who are most likely to be affected by this disease are children who are in a growth spurt, especially boys who are from the ages of 5 to 13 years old. 60% of children with Sever’s disease have both heels involved.
Symptoms of this disease are heel pain that intensifies during running and jumping activities. The pain is typically localized to the posterior part of the heel. Symptoms may be severe, and they can easily interfere with daily activities. Children who play soccer, baseball, and basketball are more likely to develop Sever’s disease.
Your doctor will diagnose your child based on his or her symptoms, x-rays are generally not helpful in diagnosing this disease. Your doctor may examine both heels and ask your child questions about his or her activity level in sports. Your doctor may then use the squeeze test on your child’s heel to see if there is any pain. Nevertheless, some doctors might still use x-rays to rule out any other issues such as fractures, infections, and tumors.
Sever’s disease can be prevented by maintaining good flexibility while your child is growing. Another prevention method is to wear good-quality shoes that have firm support and a shock-absorbent sole. Sever’s disease can be treated by ceasing any activity that causes heel pain. You should apply ice to the injured heel for 20 minutes 3 times a day. Additionally, orthotics should be used for children who have high arches, flat feet, or bowed legs.
If you suspect your child has Sever’s disease, you should make an appointment with your podiatrist to have his or her foot examined. Your doctor may recommend nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen to relieve pain. In more severe cases, your child may need a cast to rest his or her heel. Fortunately, Sever’s disease does not cause long-term foot problems. After treatment, your child should start to feel better within two weeks to two months.
Psychological Effects of Toenail Fungus

Onychomycosis, commonly known as toenail fungus, is the most prevalent nail disorder, with a growing incidence, particularly among the elderly. This condition is notorious for its stubbornness, requiring prolonged and often ineffective treatments, with frequent recurrences. Beyond affecting the nail's normal function, fungal nail infections can bring pain, an unsightly appearance, disruption of daily life, and negative psycho-social consequences. Patients often grapple with embarrassment, diminished self-esteem, and social withdrawal due to toenail fungus. Recent advances in treatment have emerged, offering more effective solutions. If you suffer from toenail fungus, it is suggested that you make an appointment with a podiatrist to discuss the physical and psychological effects of this condition. Honesty with this medical professional about how much it impacts your life is important in obtaining a more holistic approach to treatment.
For more information about treatment, contact the podiatrists of Issaquah Foot & Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact one of our offices located in Issaquah, WA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
Footwear Influence on Bunions

Bunions, or hallux valgus, is a foot deformity where the big toe tilts toward the second toe, causing a bony lump on the side of the foot. Symptoms include pain, swelling, callused skin, and changes in foot shape. Contrary to popular belief, fashion shoes such as high heels do not directly cause bunions. Bunions are primarily the result of a genetic predisposition and the mechanical structure of the foot. However, wearing shoes that squeeze the forefoot and crowd the toes can worsen an existing condition and lead to pain and joint deformity. Bunions can also develop due to factors such as age, arthritis, or sports activities. Preventing bunions involves choosing sensible, well fitting footwear with ample toe room. Avoiding pointed shoes and excessive heels can be helpful. Proper footwear, non surgical treatments and wearing orthotics are initial choices. Surgery is typically the last option for bunions causing significant pain. This involves removing the bony lump and realigning the big toe, ultimately improving foot function and comfort. If you have a bunion that is causing discomfort, it is suggested that you make an appointment with a podiatrist to have it evaluated and obtain appropriate treatment.
If you are suffering from bunion pain, contact the podiatrists of Issaquah Foot & Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Issaquah, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
Types and Causes of Broken Toes

A broken toe, though seemingly minor, can cause significant pain and disruption to daily life. The types and causes of these kinds of fractures encompass a range of scenarios. First, a common cause of a broken toe can happen when the toe is stubbed against a hard surface, and is often classified as a traumatic break. Second, stress fractures, which can result from repetitive impact, can occur, particularly in athletes or people who engage in rigorous physical activities. Fractures due to osteoporosis may also cause a broken toe, especially in the elderly. Vigorous activities, accidents, falls, and even dropping heavy objects onto the foot are common triggers for toe fractures. Recognizing the types and understanding the causes of broken toes is vital in seeking timely medical attention and implementing precautionary measures to prevent these painful disruptions. If you have broken your toe, it is suggested that you consult with a podiatrist who can accurately diagnose toe fractures and guide you toward the treatment method that is correct for you.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact the podiatrists from Issaquah Foot & Ankle Specialists. Our doctors will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact one of our offices located in Issaquah, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What to Know About a Broken Toe
Trauma to the foot, especially the toes, can occur in many ways. Banging them, stubbing them, or dropping something on them are a few different ways this trauma can occur. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break or fracture. Another type of trauma that can break a toe is repeated activity that places stress on the toe for prolonged periods of time.
Broken toes can be categorized as either minor or severe fractures. Symptoms of minor toe fractures include throbbing pain, swelling, bruising on the skin and toenail, and the inability to move the toe with ease. Severe toe fractures require medical attention and are indicated when the broken toe appears crooked or disfigured, when there is tingling or numbness in the toe, or when there is an open, bleeding wound present on the toe.
Generally, a minor toe break will heal without long-term complications. However, it is important to discontinue activities that put pressure on the toe. It is best to stay off of the injured toe and immediately get a splint or cast to prevent any more additional movement of the toe bones. You can also immobilize your toe by placing a small cotton ball between the injured toe and the toe beside it. Then, tape the two toes together with medical tape. Swelling can be alleviated by placing an ice pack on the broken toe directly as well as elevating your feet above your head.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery, especially when the big toe has been broken. Due to its position and the pressure the big toe endures with daily activity, future complications can occur if it is not properly treated. Pain associated with minor toe fractures can be managed with over-the-counter pain medications. Prescription pain killers may be necessary for severe toe fractures.
The healing time for a broken toe is approximately four to six weeks. In severe cases where the toe becomes infected or requires surgery, healing time can take up to eight weeks or more. While complications associated with a broken toe are immediately apparent, it is important to note that there are rare cases when additional complications, such as osteoarthritis, can develop over time. You should immediately speak with your podiatrist if you think you have broken your toe due to trauma. They will be able to diagnose the injury and recommend the appropriate treatment options.
Foot Surgery for Rheumatoid Arthritis May Improve Mobility

Rheumatoid arthritis, abbreviated RA, is a chronic autoimmune condition that can severely impact the joints, including those in the feet. When conservative treatments fail to provide adequate relief, foot surgery becomes a viable option for managing RA and related foot deformities. Surgical procedures aim to correct joint alignment, reduce inflammation, and improve overall foot function. Common surgical interventions for RA in the feet include a synovectomy, which is the removal of the inflamed joint lining, tendon repair or transfer, joint fusion, and joint replacement. It's important to note that foot surgery for RA is considered a last resort when other treatments have proven ineffective. It is beneficial for patients to work closely with their podiatrist to determine the most suitable surgical approach based on individual needs and medical history. While foot surgery may involve a recovery period, it can significantly enhance mobility, reduce pain, and ultimately improve the quality of life for those living with RA. It is suggested that you consult with a podiatrist if this condition affects you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact the podiatrists of Issaquah Foot & Ankle Specialists. Our doctors will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact one of our offices located in Issaquah, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.