Achilles Tendon Bursitis
Achilles tendon bursitis is a painful condition that involves inflammation of the fluid filled sac, or bursa, located between the skin of the heel. Posterior Achilles tendon bursitis affects the back of the heel, while anterior Achilles tendon bursitis, also called retromalleolar bursitis, is felt in front of the attachment of the Achilles tendon to the heel bone. Symptoms include swelling, warmth, pain, and a tender spot at the back of the heel. Diagnosis by a podiatrist begins with a discussion of symptoms and a medical history, followed by a physical examination to identify signs of inflammation and tenderness. X-rays may be used to rule out other potential causes of heel pain, and in some cases, an ultrasound or MRI may provide more detailed views. The primary goal is to relieve inflammation and reduce pain. Treatment approaches may vary based on the severity and location of the pain. In rare cases, surgical intervention may be considered. For help in relieving the pain of Achilles tendon bursitis, it is suggested that you make an appointment with a podiatrist.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact the podiatrists of Issaquah Foot & Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
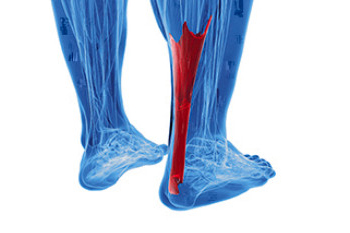
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Issaquah, WA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
Kidney Disease and Foot Ulcers
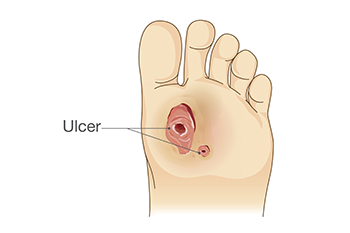
Kidney disease is a serious condition that can give rise to foot problems, primarily due to nerve and blood vessel damage. Two significant complications related to kidney disease and foot health are circulation issues and altered sensation. These changes can develop gradually, often without noticeable symptoms. One common foot problem associated with kidney complications is a foot ulcer, where the skin breaks down, exposing underlying tissue. Unfortunately, the skin's poor healing ability in some kidney disease patients makes them more susceptible to ulcers or infections, even from minor injuries. These foot ulcers can become infected, and if left untreated, may lead to severe complications, including an increased risk of heart attacks and strokes. If you have kidney disease, it is suggested that you are under the care of a podiatrist to set up regular screenings and assessments to detect any potential issues early and create a personalized treatment plan.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact the podiatrists from Issaquah Foot & Ankle Specialists. Our doctors will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact one of our offices located in Issaquah, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Systemic Diseases of the Foot
There are several systemic diseases, or diseases that affect the whole body, that either display symptoms in the feet or affect the health of the feet. Common systemic diseases that affect the overall health of the feet, and the patient’s ability to walk comfortably, include gout, diabetes mellitus, neurological disorders, and arthritis, among others.
In gout, which is caused by an excessive buildup of uric acid in the body, the most common symptoms of pain, inflammation, and redness occur at the metatarsal/phalangeal joint at the base of the big toe. Any excess levels of uric acid crystallize and are deposited in tendons, joints, and surrounding bone and muscle tissue. Gout is commonly treated with NSAIDs to relieve pain and inflammation and other drugs to lower uric acid levels in the body. Gout most commonly affects those who are overweight, have low protein diets and lead a more sedentary lifestyle.
Diabetes mellitus is an increase in the level of blood sugar in which the body cannot counteract with naturally occurring insulin in the body. The three types of diabetes, Type I, Type II and Gestational Diabetes, are all signs the body is either not producing enough insulin or is not efficiently using the insulin that is produced. Gestational diabetes only affects women who are pregnant and have never, prior to pregnancy, exhibited symptoms of the disease.
There are two main issues that affect the feet that are commonly caused by diabetes. They include diabetic neuropathy and peripheral vascular disease. Diabetic neuropathy can lead to damaged nerves and affect the feet through numbness and loss of sensation. Peripheral vascular disease restricts the flow of blood to the foot and can, in extreme cases, lead to the necessity of amputating the foot. Peripheral issues that are caused by diabetes and can affect the foot include athlete’s foot, nail infections, corns, blisters, bunions, severe dry skin, plantar warts and ingrown toenails. These can all be attributed to the decrease of blood flow to the foot.
Neurological disorders and rheumatoid arthritis can also have severe impact on the health of the feet. Neurological disorders can affect the nerves in the main structure of the foot and cause loss of sensation and possible decreased muscle response. Rheumatoid arthritis can affect the bones and joint structures of the foot, making it impossible to walk normally without serious pain.
All systemic diseases that affect the foot can effectively be treated to minimize joint and muscle damage if they are diagnosed early and treated with medication and lifestyle therapy. Diabetes patients must monitor their blood sugar levels and work with their physician to keep their levels as close to normal as possible. Rheumatoid arthritis patients should work with their physician to ensure the proper medications are being taken to reduce the amount of damage to the joints of the body.
Definition and Symptoms of Athlete’s Foot

Athlete's foot, a common fungal infection of the skin, often affects the spaces between the toes. This condition is caused by various fungi, including trichophyton and epidermophyton, thriving in warm and moist environments such as locker rooms and swimming pool areas. Symptoms typically manifest as redness, itching, and a burning sensation, particularly between the toes. As the infection progresses, the skin may peel, crack, or develop blisters, contributing to discomfort. Athlete's foot can extend to the soles of the feet, causing scaling and thickening of the skin. In severe cases, the infection may spread to the toenails, leading to additional complications. Recognizing these symptoms is important for early intervention, as untreated athletes' foot can persist and potentially spread to other parts of the body. If you have symptoms of athlete’s foot, it is suggested that you contact a podiatrist who can offer you correct treatment options, which may include prescribed medicine.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact the podiatrists from Issaquah Foot & Ankle Specialists. Our doctors will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact one of our offices located in Issaquah, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete's Foot
Athlete’s foot is an extremely contagious infection caused by a fungus that results in itching, burning, dry, and flaking feet. The fungus that causes athlete’s foot is known as tinea pedis and thrives in moist, dark areas such as shower floors, gyms, socks and shoes, commons areas, public changing areas, bathrooms, dormitory style houses, locker rooms, and public swimming pools. Athlete’s foot is difficult to treat as well because of the highly contagious and recurrent nature of the fungus.
Tinea is the same fungus that causes ringworm, and is spread by direct contact with an infected body part, contaminated clothing, or by touching other objects and body parts that have been exposed to the fungus. Because the feet are an ideal place for tinea to grow and spread, this is the most commonly affected area. It is, however, known to grow in other places. The term athlete’s foot describes tinea that grows strictly on the feet.
The most commonly infected body parts are the hands, groin, and scalp, as well as the feet. Around 70% of the population suffer from tinea infections at some point in their lives, however not all of these cases are athlete’s foot. Just like any other ailment, some people are more likely to get it than others, such as people with a history of tinea infections or other skin infections, both recurring and non-recurring ones. The extent to which a person experiences regrowth and recurrent tinea infections varies from person to person.
Sometimes people will not even know that they are infected with tinea or that they have athlete’s foot because of a lack of symptoms. However, most experience mild to moderate flaking, itching, redness, and burning. However, some of the more severe symptoms include cracking and bleeding skin, intense itching and burning, pain while walking or standing, and even blistering.
Because of the recurring nature of the tinea fungus and the athlete’s foot it causes, the best way to treat this condition is with prevention. You can take some preventative measures such as wearing flip flops or sandals in locker rooms and public showers to reduce contact with the floor. It also helps to keep clean, dry feet while allowing them to breathe. Using powders to keep your feet dry is a good idea, as well as keeping your feet exposed to light and cool air, to prevent the growth of tinea. If you do happen to get athlete’s foot, opt for using topical medicated creams, ointments or sprays. These treatments help eliminate and prevent it from coming back.
Understanding the Definition and Causes of a Bunion

A bunion, a common foot deformity, is characterized by the gradual misalignment of the big toe joint, causing a bony protrusion on the side of the foot. This condition develops when the big toe consistently pushes against the next toe, gradually altering the joint's structure. Wearing ill-fitting footwear, particularly tight shoes or high heels, is a primary culprit, as they force the toes into unnatural positions. Genetic factors also play a role, with some individuals inheriting a predisposition to bunions. Foot mechanics, such as overpronation or flat feet, contribute to the misalignment, increasing the risk. Arthritis, particularly inflammatory types, may exacerbate bunion formation. Additionally, trauma or injury to the foot can accelerate the development of bunions. Recognizing the multifaceted causes of bunions is important for preventive measures. If you have developed a bunion, it is suggested that you schedule an appointment with a podiatrist who can offer you effective relief techniques.
If you are suffering from bunions, contact the podiatrists of Issaquah Foot & Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact one of our offices located in Issaquah, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Turf Toe Can Be a Painful Foot Condition

Turf toe is a specific type of injury that primarily affects the big toe. It is a sprain of the metatarsophalangeal, or MTP joint, which connects the big toe to the foot and can result in toe pain. The name turf toe is derived from its common occurrence in athletes who play on artificial turf surfaces, but it can affect anyone. This injury typically occurs when the toe is hyperextended, causing damage to the ligaments and tendons that support the MTP joint. Symptoms of turf toe include pain, swelling, and limited range of motion in the affected toe. In some cases, there may be bruising as well. Turf toe can be a painful and debilitating condition, and often requires medical attention from a podiatrist. If you have endured this type of injury, it is strongly suggested that you are under the care of this type of doctor who can effectively diagnose and treat the cause of this toe pain.
Toe pain can disrupt your daily activities. If you have any concerns, contact the podiatrists of Issaquah Foot & Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact one of our offices located in Issaquah, WA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.