What is ESWT?
Extracorporeal shockwave treatment, also known as ESWT, is a non-invasive, non-surgical treatment option for the intense, persistent heel pain associated with chronic plantar fasciitis and achilles tendonitis. "Extracorporeal" means "outside the body." Shockwaves, also known as pressure or sound waves, are generated from a special ESWT device and focused onto the targeted tissue. The shockwaves are delivered outside the body to trigger an individual's own repair mechanisms. The concept behind shockwave therapy in orthopedic disorders is that the shockwave stimulates and reactivates healing to encourage revascularization and other elements necessary to advance normal tissue healing. Additionally, shockwaves help to over-stimulate pain transmission nerves, which can lead to a reduction in sensitivity and pain.
What is plantar fasciitis?
The plantar fascia is a band of connective tissue on the plantar surface of the heel that plays a large role in maintaining the normal architecture of one's foot. Plantar fasciitis is a common clinical condition caused by overuse or injury of the plantar fascia and is defined as traction degeneration of the plantar fascial band at its origin on the medial tubercle of the calcaneus. Inflammation, fibrosis and decreased vascularization of the fascia occur, causing symptoms of heel pain. Other symptoms that may occur include burning in the sole of the foot, recurring foot pain that is especially aching in the morning or after sitting or heel pain after beginning a new exercise routine.
What causes plantar fasciitis?
There are a number of predisposing factors, including foot pronation, obesity, poor fitting shoes, minor trauma, occupational risks and change in exercise program. Although everyone is at risk, plantar fasciitis is most commonly found in athletes, runners, overweight individuals or those who are required to stand on hard surfaces for prolonged periods of time. Although approximately 2,000,000 Americans suffer from plantar fasciitis, ESWT is an appropriate treatment option in approximately 5 to 10% of those cases, as the remainder of the cases can be adequately addressed with more conservative therapies.
Who should receive ESWT for plantar fasciitis?
Prior to undergoing ESWT treatment, the patient must have been diagnosed with chronic plantar fasciitis for at least six months. Only after the patient's symptoms fail to respond to three conservative treatments should ESWT be administered. Conservative treatments include rest, physical therapy, heel cushions, non-steroidal anti-inflammatory drugs (ibuprofen, acetaminophen, etc.), cortisone injections, taping, orthotics, shoe modifications, night splinting and casting. In years past, surgical intervention for chronic plantar fasciitis was required when these other treatments had failed. Today, ESWT is available as an alternative, non-invasive treatment option.
Who should not receive ESWT treatment for plantar fasciitis?
Your health history should be reviewed with your doctor to see if this treatment is appropriate for you. ESWT is not recommended for patients with certain conditions. Patients with pacemakers and patients taking medications that may prolong or interfere with blood clotting (coumadin) are not candidates for ESWT. Also, children or pregnant women are not considered appropriate candidates for ESWT. ESWT is not appropriate for individuals suffering from acute plantar fasciitis.
What are the side effects of ESWT?
Compared to surgery, ESWT has fewer side effects and a much shorter recovery time. The most common patient complaint is some minor pain or discomfort during and after treatment. Other side effects might include minor skin bruising, reddening or swelling of the treated area. However, these possible occurrences usually resolve within a few days. The risks associated with surgery and general anesthesia are eliminated.
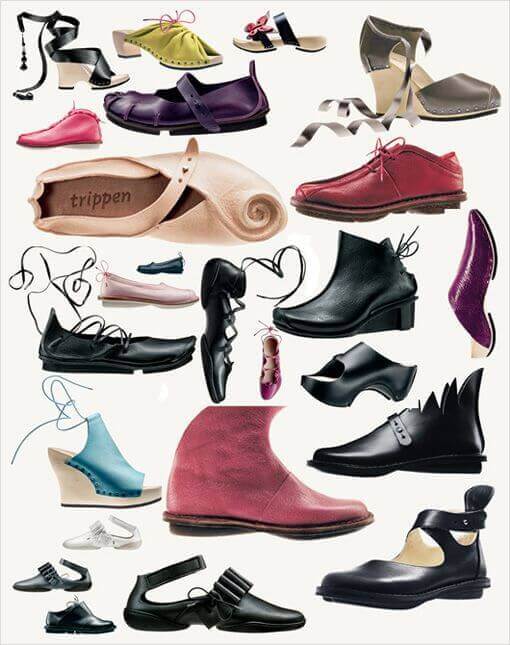 You can develop a foot or toe problem such as a bunion, plantar fasciitis, callus or hammertoe for a number of reasons, but your footwear can play a large role in how bad your foot condition becomes.
You can develop a foot or toe problem such as a bunion, plantar fasciitis, callus or hammertoe for a number of reasons, but your footwear can play a large role in how bad your foot condition becomes. 






