bfdadmin
bfdadmin
Dr. Brandon Nelson, A Double Board Certified Foot Physician & Surgeon, Issaquah’s Top Podiatrist, Discusses Bunion Surgery

Bunions can be quite painful and become a hindrance to everyday life. While there are some conservative measures that may provide some temporary relief the only long term solution is surgery.
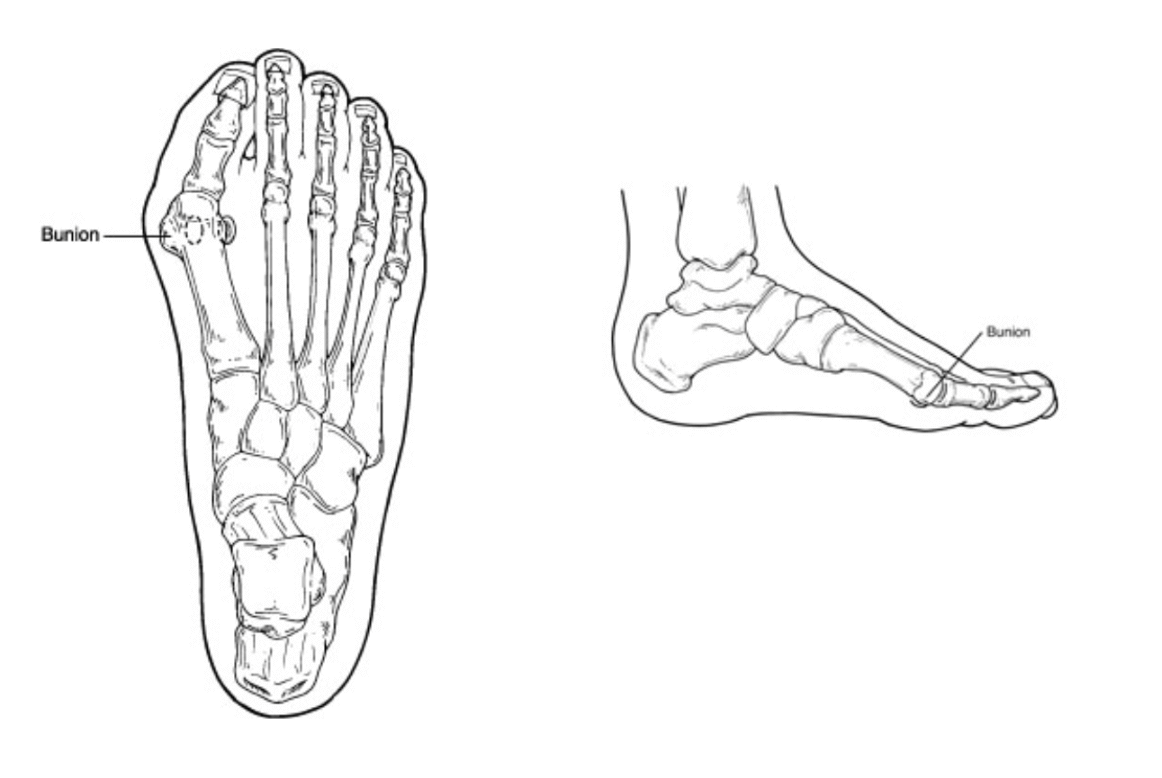
First it is important to understand what a bunion is. A bunion is when the 1st metatarsal shifts out of place. This shifting gets worse with time and the bunion gets bigger. The visual result is the big toe starts to overlap the 2nd toe and the protuberance you see at the base of the big toe is the 1st metatarsal. To fix the bunion the 1st metatarsal needs to be realigned.
The realignment of the 1st metatarsal can happen in two ways. The first being you cut the bone and reposition it anatomically. This is probably the most common bunionectomy performed in the United States. It usually involves about 4-6 weeks in a walking boot and has great outcomes for smaller bunions. The next most common would be a fusion of the tarsometatarsal joint. This is a procedure that is for larger bunions or people with unstable foot structures. This surgery usually requires a period of non-weight bearing for 3-6 weeks. Both of these procedures can have great outcomes when utilized appropriately.
How do you know which bunion surgery is best for your foot? There are many factors to take into account. The overall foot structure, any other foot pathologies, lifestyle, recovery and age. I recommend seeing a foot and ankle doctor that operates on a lot of bunions.
If you have a bunion and would like a consultation I can help. Please call 425-391-8666 or make an appointment online with Dr. Nelson.
Sincerely,
Board Certified Physician & Surgeon
Issaquah’s Top Podiatrist & Foot/Ankle Surgeon
Dr. Timothy Young, a Board-Certified Foot Surgeon discusses: Understanding Why Bunions Can Reoccur.

Bunions are a common foot condition that can cause pain, discomfort, and difficulty with footwear. They typically develop when the joint at the base of the big toe becomes misaligned, leading to a bony bump on the side of the foot. Although surgical correction can provide relief for many individuals, some individuals may find that their bunions come back or reoccur over time. Understanding the factors that contribute to bunion recurrence can help individuals take steps to prevent this from happening.
1. Genetics and Foot Structure
One of the primary reasons bunions can reoccur is because of genetics and foot structure. Some individuals are predisposed to developing bunions because of inherited foot shapes or structural conditions. Even after surgical correction, the underlying foot structure is still there and may still contribute to the gradual return of the bunion over time. A perfect example this is a juvenile onset bunion. We see patients who are teenagers who already have quite pronounced bunions. In this case they certainly inherited foot structure that makes them highly prone to this. This is commonly due to an underlying foot structure called metatarsus adductus. Pronation is another foot structure that is prone to bunions. The combination can be especially challenging, a pronated foot with metatarsus adductus.
2. Improper Footwear
Wearing tight, pointed, or high-heeled shoes can exacerbate bunion formation and contribute to their recurrence. These types of footwear by raising the heel cause extra pressure on the entire forefoot and place excessive pressure on the toes and can force the big toe joint out of alignment. Even after surgery, if individuals continue wearing these type of shoes, it can increase the likelihood of bunions coming back.
3. Post-Surgical Care
Proper post-surgical care is critical for preventing bunion recurrence. Following your surgeon's instructions regarding activity levels, wearing orthotic devices or splints, and attending follow-up appointments is essential. Failure to adhere to post-operative care guidelines can increase the risk of the bunion returning.
4. Joint Instability
In some cases, joint instability can contribute to bunion recurrence. This may occur if the surgical correction did not adequately address underlying joint laxity or if there are other issues with the foot structure and foot biomechanics. Physical therapy and exercises to strengthen the foot and improve stability can be beneficial in these situations. Note that in example this would be a round first metatarsal head with laxity of the underlying capsule and ligaments.
5. Lifestyle Factors
Certain lifestyle factors, such as obesity or activities that place repetitive stress on the feet, can also contribute to bunion recurrence. Excess weight can put additional strain on the feet and exacerbate bunion formation. Similarly, activities that involve repeated bending or pressure on the toes can lead to joint misalignment over time.
6.
Surgical factors: when I see patients who come in for a 2nd opinion and have had surgery previously and there has been recurrence, I look to see how much correction was done initially. Sometimes there is a lack of adequate correction from the beginning and this creates a higher risk of recurrence. It is important to fully correct the bunion whenever possible. For example a juvenile onset bunion needs the most corrective surgery possible because they are so prone to reoccurrence. This often means a Lapiplasty or similar procedure. Another example would be a lack of adequate release of the soft tissue at the great toe joint. It is very important that after surgery the great toe joint lines up correctly and the big toe doesn't want to pull to the side toward the 2nd toe. If the soft tissue capsule is not adequately released this can be a problem.
Preventing Bunion Recurrence
While some factors contributing to bunion recurrence are beyond individual control, there are steps individuals can take to reduce the risk:
Choose Proper Footwear: Opt for shoes with a wide toe box, low heels, and adequate arch support to reduce pressure on the toes. Hold off on the really dressy shoes except for special occasion like a wedding or a special dinner out. And even then avoid a really high heel shoe.
Maintain a Healthy Weight: Maintaining a healthy weight can alleviate strain on the feet and joints.
Follow Post-Surgical Care Guidelines: Adhere to your surgeon's recommendations for post-operative care, including wearing orthotics and attending follow-up appointments.
Monitor Foot Health: Regularly check your feet for any signs of bunion recurrence or other foot issues, and seek medical attention if necessary.
Consider Conservative Treatments: In some cases, conservative treatments such as orthotics, padding, and physical therapy may help prevent bunion recurrence or delay its progression.
For those very high-risk patients using a "retainer" similar to a dental retainer can be used to help maintain the alignment of the great toe and keep it from drifting toward the 2nd toe or at least really slow its progression.
Make sure to discuss this concern if you are in for a surgical consultation. If you would like a 2nd opinion or have additional questions and would like consultation at our clinic, I would be happy to provide this consultation.
By understanding the factors that contribute to bunion recurrence and taking proactive measures, individuals can help reduce the likelihood of experiencing this common foot problem again in the future.
If you have any questions or would like a consultation please call 425-391-8666 and make an appointment online.
Dr. Timothy Young
Foot & Ankle Surgeon
Issaquah's Top Podiatrist
Dr. Brandon Nelson, A Double Board Certified Foot Physician & Surgeon, Issaquah’s Top Podiatrist, Discusses Your Bunion
Bunions are often looked at as just a cosmetic concern however this is not true. They can cause pain and discomfort and lead to more foot problems in the future. Today I will discuss bunions, what they are, their cause, symptoms and what we can do to treat them.
What is a bunion?
A bunion is a bony protrusion of the 1st metatarsal. It occurs as the 1st metatarsal shifts out of place and the big toe begins to drift towards the second. This begins as a small misalignment of the joint and grows larger and more malaligned as time and mileage increase.
Causes of bunions:
There are many causes of bunions and from long term research we know the following are the most common.
-Genetics plays a large role in the development of a bunion. You inherit your foot structure and this can predispose you to a bunion.
-Another source cited is footwear. Anything that puts more forefoot pressure like a high heeled shoe can accelerate bunion formation.
-Systemic causes can be attributed to bunions. Conditions like Rheumatoid arthritis or other arthropathies that attack joints.
Symptoms:
These are what usually bring patients into the office. These are things like having a hard time fitting shoes, rubbing the big toe on the 2nd toe. Another common symptom is pain or swelling and redness of the big toe joint.
Treatment:
I usually break the treatment up to conservative and surgical. The conservative measures include, no bare feet and wearing a wider shoe. Save your money no splints or stretching devices of the big toe work. Remember this is a bony malalignment and you can not move bones from the outside of your foot. Surgery is the only long term fix. The surgical correction depends on the size, age and overall foot structure.
If you have a bunion and would like a consultation I can help. Please call 425-391-8666 or make an appointment online, and ask for an appointment with Dr Nelson.
Sincerely,
Double Board Certified Physician & Surgeon
Issaquah’s Top Podiatrist & Foot/Ankle Surgeon
Dr Brandon Nelson, A Double Board-Certified Physician & Surgeon, Discusses Painful Hammertoes
Hammertoes are a common pathology I see in my office. Most patients with curled toes have pain with activities and a hard time fitting shoes. They describe a progression of the toes where other forefoot pathologies can be present.
The most common cause appears to be foot structure and genetics. We see patients that have flatter feet require increased pressure from the tendons in their toes to stabilize. This repetitive pressure can cause pain and discomfort. Some people will inherit a foot structure that can predispose them to hammer toes. These foot structures are ones that often develop bunions as well.
Symptoms:
The symptoms can vary from patient to patient. The most common symptoms include swelling and pain. Some patients relate a significant stiffness or bending to the toes that pushes in their shoes. All can be painful, especially with physical activities.
Treatment:
We have many options available for hammer toes. But it should be noted it is based on the degree of the hammer toe. How significant is the bending and contracture of the digit. It is important to have a good clinical evaluation and an x-ray. If you would like a consultation for your hammer toe pain I can help. Call to make an appointment with me at 425-391-8666 or make an online appointment.
Sincerely,
American College of Foot & Ankle Surgeons
Issaquah’s Top Podiatrist
Dr. Timothy Young discusses the Adductoplasty Procedure for Midfoot Arthritis: A Comprehensive Guide
What is Adductoplasty? Adductoplasty is a surgical procedure designed to treat midfoot arthritis by realigning the bones in the midfoot region. It specifically targets the midfoot joints, such as the 2nd and 3rd metatarsal cuneiform joints (also known as the tarsometatarsal joints or TMT joints), which are commonly affected by arthritis. The goal of the adductoplasty procedure is to correct deformities, alleviate pain, and improve joint function and address arthritis joint pain.
Who Can Benefit from Adductoplasty? Adductoplasty is typically recommended for individuals with moderate to severe midfoot arthritis that hasn't responded adequately to conservative treatments. Common symptoms that may indicate the need for adductoplasty include persistent pain, stiffness, swelling, and difficulty walking or bearing weight on the affected foot.
The Procedure:
- Preoperative Assessment: Before undergoing adductoplasty, patients undergo a thorough preoperative assessment, including imaging studies like X-rays or MRI scans to evaluate the extent of arthritis and deformity.
- Anesthesia: Adductoplasty is performed under general anesthesia or IV sedation type anesthesia, depending on the patient's health and surgical preferences.
- Incision and Access: The surgeon makes an incision on the affected foot to access the midfoot joints. Minimally invasive techniques may be used to minimize tissue damage and promote faster recovery.
- Bone Realignment: Using specialized instruments, the surgeon realigns the bones in the midfoot to correct deformities and restore proper joint alignment. This will involve removing damaged cartilage or bone spurs.
- Stabilization: Additional procedures like joint fusion are necessary to stabilize the joint and promote healing.
- Closure and Recovery: Once the procedure is completed, the incision is closed, and the foot is bandaged. Patients are monitored in the recovery room before being transferred to a hospital room or discharged home, depending on the surgical plan.
Recovery and Rehabilitation: The recovery timeline for adductoplasty varies depending on the individual and the extent of the procedure. However, here are general guidelines:
- Postoperative Care: Patients are advised to keep the foot elevated and apply ice to reduce swelling and discomfort.
- Weight-Bearing: The surgeon will provide instructions on when and how much weight can be placed on the foot. Crutches or a walking boot may be recommended initially.
- Physical Therapy: Rehabilitation typically involves physical therapy to improve strength, flexibility, and mobility. Patients learn exercises to restore function and prevent stiffness.
- Follow-Up Visits: Regular follow-up visits with the surgeon are essential to monitor healing, address any concerns, and adjust the rehabilitation plan as needed.
Benefits of Adductoplasty:
- Pain Relief: Adductoplasty can significantly reduce pain and discomfort associated with midfoot arthritis, allowing patients to engage in daily activities more comfortably.
- Improved Function: By correcting deformities and realigning the bones, adductoplasty improves joint function, enhancing overall quality of life.
- Long-Term Results: Many patients experience long-lasting benefits from adductoplasty, especially when combined with postoperative rehabilitation and lifestyle modifications.
Conclusion: Adductoplasty is a valuable surgical option for individuals suffering from midfoot arthritis, offering pain relief, improved joint function, and enhanced quality of life. If you're considering adductoplasty or exploring treatment options for midfoot arthritis, consult with a qualified orthopedic surgeon to determine the best course of action based on your specific needs and goals. With proper care, rehabilitation, and follow-up, adductoplasty can pave the way for a more active and pain-free lifestyle.
If you have any questions or would like a consultation please call 425-391-8666 and make an appointment online.
Dr. Timothy Young
Foot & Ankle Surgeon
Issaquah's Top Podiatrist
Dr. Timothy Young discusses what to expect after Lapiplasty bunion surgery, focusing on post-op recovery.
Here are the key points:
- Day of Surgery:
- Arrival at the surgery center, where preparation and anesthesia discussions occur.
- The surgery typically lasts around 2 hours, involving incisions, bunion removal, and toe joint realignment.
- Recovery Timeline:
- Post-operative care in the recovery room with monitoring and pain management.
- Most patients go home on the same day.
- First Weeks After Surgery:
- Pain management with prescribed medication.
- Swelling and bruising are normal; ice packs and elevation help.
- Weight-bearing timeline varies, with gradual progression from non-weight bearing to partial weight bearing over weeks.
- First 2 weeks after the Lapiplasty, using a scooter or crutches and keeping weight off week 3-6 after surgery you start to progressively bear weight with your boot. For example, at the beginning of week 3 you will spend 15 minutes per hour allowing weight with the boot on your heel. The following week you'll spend 20 - 30 minutes per hour with the boot and with the final week 45 minutes per hour with the boot.
- Long-Term Recovery:
- Physical therapy may be recommended after 4-6 weeks to restore strength and flexibility.
- Driving can be as early as 6 weeks after surgery.
- Using the stationary bike and upper body workout can be done as early as week 5 - 6 after surgery.
- Gradual return to normal activities over several months. Bone healing and stability of the fusion site usually occurs after the initial 4 months. This is why it's necessary to wait for high-impact activities like jumping and running until 4 months.
- Full recovery can take six months to a year.
- Complications:
- Working closely with our patients, our goal is to avoid complications such as infection, poor wound healing, nerve damage, or bunion recurrence.
- Following post-operative care instructions is crucial to avoid these complications.
- Conclusion:
- Bunion surgery can be life-changing and literally change the structure of your foot.
- Patients should follow their surgeon's advice for a smoother recovery and embrace a more comfortable, active lifestyle with patience and proper care.
If you have any questions or would like a consultation please call 425-391-8666 and make an appointment online.
Dr. Timothy Young
Foot & Ankle Surgeon
Issaquah’s Top Podiatrist
Dr. Brandon Nelson, A Double Board-Certified Physician & Surgeon, Discusses Neuromas
Neuromas are an inflammatory disorder of the nerves in your foot. Typically, it is in the forefoot between the 3rd and 4th toe. It most commonly presents in the 3-5th decade of life and seems to be more common in women.
Causes:
The most common cause appears to be foot structure. We see patients that have a higher arched foot put a lot of pressure on their forefoot. This reparative pressure can inflame the nerves in the front of the foot causing a neuroma to form. Footwear choices can further exacerbate this, especially narrow shoes, or high heels. Other things like repetitive stress, running, jumping, anything that causes more forefoot pressure can cause neuroma pain.
Symptoms:
The symptoms can vary from patient to patient. However, some of the most common symptoms include burning, tingling and pain. Some patients relate that taking off their shoes reduces the pain and burning. Some relate rubbing helps the symptoms and some may feel a lump with rubbing of their foot.
Treatments:
We have many options available for treatment of neuromas. Some of the most common included orthotics, NSAIDS, and injections. I personally like to use dehydrated alcohol therapy it seems to have the highest success rate approaching 90%. Before treatment the most important thing is to get a correct diagnosis.
Neuromas can be very challenging and there are a few other problems that mimic neuroma symptoms. A careful diagnosis and treatment plan can be successful and not result in the need for surgical removal of the neuroma.
If you would like a consultation for your neuroma pain I can help. Call to make an appointment with me at 425-391-8666.
Sincerely,
Dr Brandon Nelson
American College of Foot & Ankle Surgeons
Issaquah’s Top Podiatrist
Dr Brandon Nelson, A Double Board-Certified Physician & Surgeon, Discusses Stubborn Heel Pain

I have to say that exercise for me helps with my mental health and overall wellbeing. I typically workout 6/7 days a week and enjoy running, biking, rucking and walking the dog. It is a great stress relief and helps me clear my head after a day of work. I am sure many of you can relate and as the weather clears more of us are getting back into an exercise routine.
That being said, I always see a spike in heel pain patients this time of year. It makes sense with the weather drying up and everyone wanted to get outside and ready for summer. Heel pain can really sideline you as you return to activities. It can come on suddenly and stick around for months. As a side note, the earlier you get treatment the faster you can recover. It is usually caused by inflammation of your plantar fascia.
The plantar fascia is the main support network of the foot. It is a soft tissue structure that runs from your heel to your toes. It has the function of controlling the foot and helping with propulsion. It can get worn out with time or tired from increased loads. It is by far the most common condition I treat.
Some patients wait quite a while before coming in and these cases are often what I call “stubborn heel pain” or “chronic fasiitis”. This is because the inflammation has now become chronic, and the body has given up on trying to fix it and now coexists with this pathology. These cases are harder to treat and usually require more extensive care. I think it is important to understand that once it becomes chronic, part of the treatment usually requires a reactivation of the body’s ability to recognize this condition. You must take the chronic state of inflammation and turn it back to an acute state.
I really enjoy helping my patients get their life back and their feet pain free. If you would like a consultation for your heel pain I can help. Call to make an appointment with me at 425-391-8666 or make an appointment online.
Sincerely,
American College of Foot & Ankle Surgeons
Issaquah’s Top Podiatrist
Dr. Brandon Nelson, A Board Certified Foot Physician & Surgeon, Issaquah’s Top Podiatrist, Discusses Why You Should Have Your Bunion Fixed

Bunions are one of the most common reasons people schedule an appointment with a foot and ankle surgeon. It is by far the most common surgical procedure I do. People of all ages and activity levels can have a bunion. The primary reason people schedule an appointment is difficulty fitting the shoes they would like to wear.
I think there are quite a few reasons to fix your bunions these days and I will discuss a few of the most beneficial reasons.
Bunions are an inherited foot disorder and are more common in women. They are usually the result of a foot that wants to flatten out too much or what we would call pronate. A bunion results when the first metatarsal tries to stabilize the medial arch. This results in the first metatarsal moving out of place and the bunion developing. Fixing a bunion can result in stabilization of the medial arch. This can have effects on the overall stability of the foot. I see patients that have had plantar fasciitis or other stability issues that resolve once the bunion is fixed.
2. Shoe Fit
Another big issue with bunions becomes an inability to fit in normal shoes. I see a lot of wide shoes and short extra depth shoes when people try to accommodate bunions and other toe deformities. It is often a relief to be able to have shoes fit again and get back to wearing the shoes you once enjoyed or liked after your toe is straightened.
3. Your Bunion Will Get Larger
Many people believe they can use straps or tape or toe straighteners and change their bunion. However, we know from long term data this is not true. There is no way to reverse your bunion without surgery. Everyone’s bunion with time and mileage will get bigger. I recommend having it fixed before it causes the 2nd toe to become a hammer toe or begins to cross over or under the 2nd toe.
If you have a bunion and want an evaluation schedule an appointment with me, or make an appointment online, I will help you.
Sincerely,
Board Certified Physician & Surgeon
Issaquah’s Top Podiatrist & Foot/Ankle Surgeon
Dr Brandon Nelson, A Double Board Certified Physician and Surgeon, Discusses Bunion Surgery Questions
Every week a few patients come in wondering about having their bunion fixed. I really enjoy these discussions and helping patients decide what is best for them. There are quite a few common questions I get so I decided to answer them in this blog
1. How much time will I need to be off my feet?
This question really depends on what procedure is utilized to correct your bunion as well as any additional procedures performed. It can be as little as a few days or up to 6 weeks. I like to get my patients walking as quickly as possible.
2. When can I start to exercise?
Again this is a tough one to answer. But, I am an avid exerciser and know how important it is to maintain our current levels and not lose too much ground with time off. I like to help my patients develop a post-operative plan to continue working out and modify activities.
3. When will I be back in a normal shoe?
This again depends on other procedures performed and how much work was needed to correct your bunion. I see some patients back in a normal shoe at 4 weeks and some as long as 10 weeks. The best thing you can do as a patient is follow your post-operative instructions.
4. Will my bunion recur?
I always recommend seeing a physician that does quite a few bunion surgeries as this will give you better outcomes. Procedure selection is the most important component to decrease recurrence rates. With proper selection recurrence rates are about 2-3%.
If you have a bunion and would like a consultation please call 425-391-8666 and make an appointment online.
Sincerely,
Foot & Ankle Surgeon
Issaquah’s Top Podiatrist